Rivka Galchen · Whack-a-Mole: Anti-Vax Sentiments · LRB 27 January 2022

Please sign in to read the full article.
–>
In the late 1840s, the Hungarian obstetrician Ignaz Semmelweis oversaw two free maternity clinics in Vienna. The clinics accepted patients on alternate days. At the first clinic the mortality rate was 10 per cent; at the second, it was 4 per cent. The clinic with the low mortality rate trained midwives. The clinic with the high mortality rate trained medical students. Fear of the medical trainees’ clinic was so great that some women chose to give birth in the street – that way they could say they had been on their way to the clinic, and still receive free medical care for their baby. Even the women giving birth in the street had lower mortality rates than those giving birth at the clinic staffed by medical students. Semmelweis set out to discover the reason for this. He concluded that the medical trainees needed to wash their hands, like the midwives did. For this, he was dismissed as a madman.
Or rather, most doctors dismissed him as a madman. At his own clinic, the students adopted the new handwashing regime. Maternal fatality rates dropped dramatically. Semmelweis presented this evidence to the world. Again, his findings were rejected. When his term as clinic director ended, he wasn’t re-hired. He returned to his native Budapest, where he had to ask around even for poorly paid work (he eventually became professor of obstetrics at the University of Pest). He wrote a book on his research, hoping that, with all the data and arguments assembled, others would see what he saw. The book received poor reviews. He was portrayed as a man in the grip of an obsession, a man who wouldn’t stop talking about dying women.
He started drinking heavily. Even his wife began to complain about his obsession. He was often seen with a prostitute. He may have developed neurosyphilis, but this remains unclear. The maddening effects of professional and social rejection can’t have helped his mental state. In the summer of 1865, he was committed to an asylum, where he was beaten by the guards. He died shortly afterwards from infected wounds. Those infections could probably have been prevented if the guards had washed their hands. Mortality rates at the maternity clinics rose again after the handwashing regime was abandoned. Only some years later, in Germany, did it become common practice for doctors to wash their hands (they used chlorine).
In her introduction to Stuck: How Vaccine Rumours Start – and Why They Don’t Go Away, Heidi Larson describes her time as Unicef’s strategy and communications director for new vaccines, which overlapped with the 2003-4 boycott of the organisation’s polio programme in northern Nigeria. Rumours had spread that the vaccines caused sterility in children. During the fourteen months of the boycott, the Nigerian strain of the virus found its way to other African countries and then, via the Hajj, as far afield as Indonesia. Larson recognised the power of the rumours, and she also recognised that the fact they were untrue, and could be proved so, was an insufficient counterweight to that power. Her book, mostly written before the current pandemic, looks at what she calls the ‘ecology of rumours’. She argues that ‘understanding the contagion of not just viruses but also sentiments and beliefs is crucial to the future of vaccines.’
In the case of the polio vaccine, a candidate from northern Nigeria had lost to a southern candidate in a tense presidential election. A northern state governor responded by calling for a boycott of the Unicef programme, harnessing pre-existing (and widespread) distrust of the West. Northern Nigeria is predominantly Muslim, while the south is predominantly Christian. It wasn’t a huge leap to imagine that the Christian south might be collaborating with Western powers to limit population growth in the north. All attempts by the federal government to dispel the rumours through reports by technical committees failed. Eventually the boycott was ended after dialogue with political and religious leaders in the north; and after the leaders of the boycott observed the vaccine being tested in Muslim countries. The rumours still resurface.
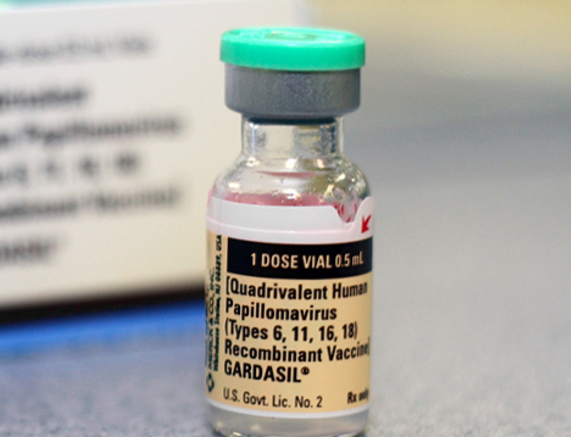
Larson left Unicef in 2005, worked for a time at Harvard’s Centre for Population and Development, and then founded the Vaccine Confidence Project, an interdisciplinary research group based at the London School of Hygiene and Tropical Medicine. Her goal was to develop a system to ‘detect the emergence, evolution and impacts of vaccine rumours’ that might replace the ineffective attempt to debunk rumours one by one she had observed in the field (the ‘whack-a-mole’ approach). Facts, as Semmelweis found out, are poor foot soldiers. One of Larson’s case studies concerns the roll-out in Carmen de Bolívar in Colombia of the HPV vaccine, which helps prevent cervical cancer caused by the human papillomavirus. In May 2014, fifteen teenage girls in the town were hospitalised with mysterious symptoms: a racing heart, shortness of breath and numbness in the arms and legs. Suspicion fell on the HPV vaccine they had received a few months earlier. (Associated as it is with a sexually transmitted disease, and administered mostly to young women, the HPV vaccine has been an alembic for all sorts of fear and anxiety around female sexuality.) In the weeks following the initial hospitalisations, another 75 girls from the same school came forward with similar symptoms; before long, five hundred girls in the area claimed to be affected. A medical team was sent to investigate. Was it the water, the food? The area’s history of violence and abuse? The vaccine?
The team concluded it wasn’t the vaccine. They labelled it a ‘mass psychogenic reaction’. Psychosomatic illness is real; but it has also been used to dismiss diseases with biological causes, especially in women (including morning sickness and PMS). Calling symptoms ‘psychosomatic’ generally doesn’t go down well. It didn’t go down well in Colombia. As in Nigeria, the situation had arisen around the same time as a contentious presidential election. After President Juan Manuel Santos, fighting for re-election, announced that there was no link between the mysterious illness and the vaccine, his health minister arrived in Carmen de Bolívar to find a crowd of furious protesters waiting. The number of girls receiving the HPV vaccine in Colombia declined dramatically.
What could have been done differently? Discounting the concerns of anxious parents may not work, but listening to them, or seeming to, can cause more harm. In 1998, the French government temporarily suspended a school Hepatitis B vaccination programme to reassure the public that it was taking seriously (spurious) concerns about a link to multiple sclerosis. Vaccination rates fell, and even French doctors were confused. The vast majority reported being ‘unsure’ about the vaccine’s safety; two-thirds said they were no longer sure of its effectiveness. Something similar happened in Japan in 2014. In response to scientifically unfounded concerns raised by mothers’ groups, the government downgraded its HPV vaccination policy from ‘proactive’ to ‘available on request’. The uptake among school-age girls fell from 70 per cent to 0.3 per cent. There is global scientific consensus that the HPV vaccine, like the Hep. B vaccine, is safe and effective.
Right-wing politicians have proved skilled at piggybacking on the populist power of anti-vax sentiments. In Italy, the far-right Five Star Movement used a vaccine mandate introduced by the centre-left coalition in 2016 to increase its own visibility, repeating false claims about proven vaccines. After the 2018 election, which brought the M5S to power, its health minister, Giulia Grillo, fired all thirty members of the government’s scientific advisory board: it was, she said, time to ‘give space to the new’. The current national unity government has reversed this position, introducing one of the toughest vaccine passport regimes in response to Covid: a ‘super green’ pass, signalling double vaccination, is required in most public places. People aged over fifty have to be fully vaccinated in order to work, as do most government employees.
One success of the anti-vax movement is that we now spend so much time talking about it. In his book Anti-Vaxxers: How to Challenge a Misinformed Movement, Jonathan Berman notes that in the US the group of the ‘under-vaccinated’, which consists mostly of minorities and the poor, is far bigger than that of the ‘anti-vaxxers’, who are primarily, though not exclusively, wealthy white women (Covid has, obviously, changed this). His book, which was also completed before the pandemic, sees the internet as the misinformation machine. A study from 2008 showed that – even by that date – half of all search results for ‘vaccine safety’ and ‘vaccine danger’ gave incorrect information, and that a quarter of the websites offering false information imitated the look of official organisations, inaccurately framed vaccination as a matter of debate within the medical community, or presented themselves as sources of ‘unbiased’ information. More recent studies, particularly of Twitter, have shown that scare stories spread further and faster than reliable data.
Berman points out that although false claims about vaccines shift over time and sometimes morph rapidly, they usually fall under one of the categories established by an anti-vaccination pamphlet in the mid 19th century: bodily pollution, personal liberty and scepticism of the science. The pamphlet was published in response to the national vaccine mandate imposed by the British government in 1853 to curb the spread of smallpox. A form of vaccination known as variolation had been practised for at least three centuries. In the Mughal Empire, smallpox fluid and powdered smallpox scabs were inhaled to provoke immunity. In Europe, rural families sent their children to variolation ‘barns’ where they were infected with smallpox via scratches to the skin. The resulting illness was usually localised and less severe: around one in thirty children died, as opposed to four-fifths of those who caught smallpox naturally.
It had been long observed that dairymaids tended not to catch smallpox, and their exposure to cowpox was considered a probable cause. In 1774, an English farmer called Benjamin Jesty decided to test the theory. On learning of a local smallpox outbreak, he took a darning needle, punctured the pustule on a cow infected with cowpox and then scratched himself, his wife and his children with the same needle. Not everyone thought this a good idea. ‘The boldness and novelty of the attempt produced no small alarm in the family,’ according to one doctor, ‘and no small sensation in the neighbourhood.’ The family suffered soreness and inflammation of the infected arm. But they didn’t contract smallpox.
Two decades later, Edward Jenner, a doctor and fellow of the Royal Society, went a step further. He infected a young boy with cowpox and then, two months later, with smallpox (a questionable approach, but Jenner had himself been inoculated as a child). The boy had a fever from the cowpox, but he didn’t catch smallpox. His immunity to cowpox protected him. Jenner wrote up his findings in a paper on the procedure, which he called ‘vaccination’ (from vacca, ‘cow’), and submitted it to the Royal Society in 1798. It was rejected for being, in Berman’s words, ‘too fantastical’.
The reviewing scientists expressed their revulsion at the injection of ‘beast matter’ into humans. Proponents of variolation weren’t pleased either: the ‘barns’ made handsome profits. But smallpox was so devastating and widespread that Jenner’s ideas slowly gained ground. When the breakthrough came, it was from an unexpected source: Napoleon, at war with England in 1803, vaccinated his troops. He was so pleased with the results that he awarded Jenner a medal. By 1840, the smallpox vaccine was not only accepted in England, but offered for free. Variolation was outlawed. In 1853, vaccination became mandatory for all infants under three months.
This is where the trouble began. Vaccination was new and its means were unsavoury: pus was taken from one vaccinated person to vaccinate another person, often in unsanitary conditions. This meant that other diseases were sometimes transmitted from person to person via infected needles, and vaccine sites often developed secondary infections. The relaxation a decade earlier of the laws governing dissection had made any unclaimed body (in reality, the bodies of the poor) available to medical science. Compulsory vaccination seemed to many just the latest incursion of a barbaric science. Leaders of the failed movements against the Poor Law of 1834, particularly trade unionists and factory reformers, became agitators against vaccination. Others had more mercenary motives. The increased professionalisation of medicine was threatening the business models of charlatans and doctors alike. Simple, free vaccination meant fewer patients and fewer remedies dispensed.
One consequence of anti-vaccination movements has been the incidental, or sometimes intentional, promotion of alternative (and often ineffective or dangerous) treatments. Much of the anti-vax movement today is quietly funded and fuelled by what Berman calls ‘Big Supplement’. In 1994, the US Congress exempted dietary supplements from the requirement to ‘demonstrate safety or efficacy’ that is required of drugs. At that time the industry was worth around $4 billion a year; it’s now worth almost $200 billion. In 2019, it was reported that 40 per cent of the funding for the National Vaccine Information Centre, a wildly misnamed anti-vax advocacy group, came from the osteopath Joseph Mercola, who made his fortune selling unregulated ‘natural health’ products and vitamins. The anti-vax doctor Mark Geier, quoted extensively by Robert F. Kennedy Jr in his infamous Rolling Stone article, marketed bogus autism treatments, including chelation therapy, which draws metals from the bloodstream (Geier was stripped of his medical licence in 2011). Another widely promoted autism ‘cure’ for children, Miracle Mineral Solution, is in fact the poisonous substance chlorine dioxide. Berman explains that the parasites parents are told their children will expel after ingesting the solution are ‘actually pieces of intestinal lining they had chemically burned inside their children’.
In 2010, the disgraced (but still popular on the paid-lecture circuit) anti-vaxxer Andrew Wakefield visited the Somali community in Minnesota to expound his claims that the MMR vaccine causes autism in children. In the following years, vaccination rates in this group fell from more than 90 per cent to around 50 per cent. Researchers found that the Somali community had confidence in vaccines in general, but fears that the MMR vaccine would cause their child to stop speaking persisted. In 2017, Minnesota suffered the largest measles outbreak in the state’s history. It was only when local religious leaders spoke out in favour of vaccination that rates began to rise again. The co-operation of trusted community figures did far more good than any information campaign.
Berman is keen to dispel the notion that those who refuse vaccines suffer from an information deficit problem. Anti-vaxxers collect evidence in order to disrupt or conceal the truth, not to uncover it. For those who are sceptical of vaccination without necessarily being anti-vaxxers, the most effective public health strategy remains unclear. Berman argues that ‘reactive’ responses, such as mockery, are counterproductive. He cites a series of studies that demonstrate what we might feel instinctively: showing people information that contradicts their beliefs rarely makes them change their minds, and often hardens their convictions. Factsheets like those used by the Centres for Disease Control and Prevention tend not to work, both because they are less powerful than personal narratives and because the other side produces misleading literature in the same format. Online bots and trolls are a source of both pro and anti-vax messages, in more or less equal amounts: the amount of contradictory and unstable information is as much, if not more, of a problem as the information itself.
Very few people believed there would be a vaccine in the first year of the Covid-19 pandemic. But there were two, and then three, and then many more. In the US, after the first rush to get the vaccine, the slower work of education, community outreach, lotteries, giveaways and other incentives began. A doctor in Texas told me that almost all the unvaccinated patients dying on his ICU ward hold fast to their belief that Covid is a hoax or that the vaccines are ineffective or dangerous or all of the above. The pre-existing condition is dogma. And something else, too, resulting from years of living in a country relatively free from serious diseases such as smallpox. For most people who receive them, vaccines are an unremarkable technology. We accept them because we understand the principles behind them and because we trust the data on their safety and efficacy. They don’t seem miraculous – or haven’t until recently – because the illnesses they prevent are largely absent from our lives. This is not true for much of the world, where TB and other preventable conditions continue to kill in great numbers. When the cause of milkmaids’ mysterious invincibility to smallpox was unknown, they were sometimes accused of being witches. What other explanation could there be for their persistent good health?
Send Letters To:
The Editor
London Review of Books,
28 Little Russell Street
London, WC1A 2HN
Please include name, address, and a telephone number.