How a Drug for Opioid and Alcohol Addiction Is Helping Treat Long COVID
A drug that’s helping millions of people with opioid or alcohol dependence is also being used to treat those suffering symptoms of long COVID.
Naltrexone has been around since 1984 to treat opioid or alcohol addiction. Given in high doses of 50-milligram tablets or a 380-milligram intramuscular injection, the drug works by binding to opioid receptors in the brain to block the effects—especially the urges and cravings to use—of opioids and alcohol.
Naltrexone has also been found to treat other disorders when administered in low doses. It is used off-label to treat obesity, nerve pain, anxiety, and autoimmune disorders.
“I found it very effective in my patients with rheumatoid arthritis, with Crohn’s disease, with other autoimmune processes, and chronic fatigue syndrome,” Dr. Keith Berkowitz, an internist, told The Epoch Times.
Naltrexone is given at doses of 0.5 to 4.5 milligram for patients with long COVID, along with other repurposed medications like prednisone, ivermectin, and vitamin D, according to Berkowitz. At low doses, naltrexone has a potent anti-inflammatory effect, as well as an endorphin effect.
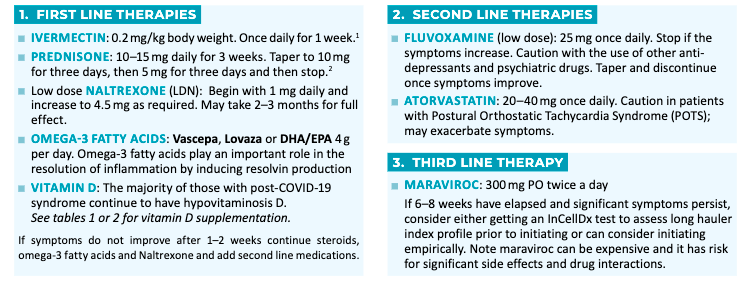
Berkowitz, who is also co-founder of the Front Line COVID-19 Critical Care (FLCCC) Alliance, said that the addition of naltrexone to the organization’s treatment protocol has been a “game-changer” for patients struggling with long COVID-19 and who have found it hard to get their symptoms taken seriously.
“I would say the majority of the patients I get [with long COVID] … they weren’t believed by someone else. I would say that’s 80 percent of the people I see,” Berkowitz said.
That’s because one of the challenges with long COVID is that there is no standard clinical definition or treatment for the syndrome. This creates difficulty for health care professionals to diagnose and treat patients with symptoms.
The World Health Organization (WHO) published a clinical case definition of long COVID as symptoms that occur in people with a “probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms and that last for at least 2 months and cannot be explained by an alternative diagnosis.”
The Centers for Disease Control and Prevention (CDC), however, defines long COVID as a “wide range of new, returning, or ongoing health problems people can experience four or more weeks after first being infected” with SARS-CoV-2, the virus that causes COVID-19.
FLCCC Alliance and other experts have recognized that long COVID may occur after an infection or receiving a COVID-19 injection.
It’s speculated that prolonged exposure to spike proteins (either from infection or an inoculation) and the lipid nanoparticle that encapsulates the messenger RNA (mRNA) produces chronic inflammation in the body, causing symptoms of long COVID.
In a study published in Circulation Research in the spring of 2021, researchers demonstrated for the first time that the spike protein was able to damage the cells of the vascular system. The study also confirmed that COVID-19 is a vascular disease rather than a respiratory illness.
“If you remove the replicating capabilities of the virus, it still has a major damaging effect on the vascular cells, simply by virtue of its ability to bind to this ACE2 receptor, the S protein receptor, now famous thanks to COVID,” Uri Manor, co-senior author of the study, said in a news release.
In a different study (pdf)—that is waiting to be peer-reviewed and published—Indian researchers examining the prevalence, predictor, and characteristics of long COVID found that people who received “two doses of COVID-19 vaccination had higher odds of developing Long COVID,” while also noting that they were not able to imply causation.
Stanford researchers, in a study published in January 2022, found that the spike protein from vaccination persisted in the body for longer than believed. The spike protein remained in lymph node germinal centers for 60 days after the second dose of an mRNA shot.
The presence of spike protein for that length of time is “highly unusual,” according to Dr. Robert Malone, who has “worked with mRNA for decades.” Malone helped develop the mRNA technology used in the COVID-19 mRNA vaccines administered around the world.
The Centers for Disease Control and Prevention (CDC) says that “after the body produces an immune response, it discards all the vaccine ingredients just as it would discard any information that cells no longer need” claiming that the spike protein doesn’t last long in the body.
“Our cells break down mRNA and get rid of it within a few days after vaccination,” the CDC said. “Scientists estimate that the spike protein, like other proteins our bodies create, may stay in the body up to a few weeks.”
Berkowitz says that the more exposure an individual has to the spike protein, the more symptoms they will likely experience.
“The one thing I have seen, the more exposure, the more symptomatic people often are,” Berkowitz said. “If they had COVID, then vaccines, and maybe COVID [again], that may be more problematic.”
Scientists aren’t sure of the exact prevalence of long COVID as they are still studying the syndrome, but it’s estimated to be between 5 percent to 80 percent. Some of the common symptoms include brain fog, joint pain, fatigue, sleep difficulties, hair loss, chest pain, and headaches.
Low Dose Naltrexone and Brain Fog


Brain fog—a term used to describe various symptoms like forgetfulness, confusion, lack of mental clarity, and poor concentration—in long COVID patients can be so debilitating that they aren’t able to work.
Cognitive dysfunction was found to be one of the most frequent persistent symptoms reported, occurring in 70 percent of long COVID patients. Brain fog, memory issues, and speech and language problems occurred more often at eight weeks or later than during initial infection, and about 86 percent of participants reported being unable to work due to cognitive dysfunction and/or memory loss, according to a study.
Researchers from the University of California–San Francisco and Weill Cornell Medicine in New York found increased levels of protein in cerebrospinal fluid in 10 of the 13 participants with cognitive symptoms who had recovered from COVID-19 but did not require hospitalization, suggesting the possibility that long COVID is due to an increase in inflammation.
In the FLCCC protocol, low-dose naltrexone, an immune modulator, is the main agent in treating symptoms of long COVID. It suppresses the inflammatory immune response by reducing the production of a certain protein, interleukin-6 (IL-6), and the inflammatory signaling pathway that IL-6 triggers.
An excessive amount of IL-6 that is not regulated is harmful to the body as it can cause neurological issues, cardiovascular effects, edema, build-up of amyloid proteins in organs or tissues, an increase in platelets (causing blood clots), and chronic autoimmune inflammation.
“Interleukin 6 (IL-6) causes a bunch of damages … and low dose naltrexone helps us modulate the interleukin 6 and nuclear factor kappa B protein, or the inflammatory pathway,” Dr. Mobeen Syed said in a video presentation on naltrexone.
Syed, the founder of DrBeen Corp, an online medical education program, says that naltrexone has to be administered in low doses for it to be effective in long COVID patients. At a dose higher than 4.5 milligrams, the drug will lose its immune-modulating effects.


