COVID-19 conspiracy ideation is associated with the delusion proneness trait and resistance to update of beliefs | Scientific Reports
Ball, P. & Maxmen, A. The epic battle against coronavirus misinformation and conspiracy theories. Nature 581, 371–374. https://doi.org/10.1038/d41586-020-01452-z (2020).
Gross, M. Recovering a sense of reality. Curr. Biol. 31, R1–R3 (2021).
Miller, B. L. Science Denial and COVID conspiracy theories: Potential neurological mechanisms and possible responses. JAMA 324, 2255–2256. https://doi.org/10.1001/jama.2020.21332 (2020).
Freeman, D. et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol. Med. https://doi.org/10.1017/S0033291720001890 (2020).
Maftei, A. & Holman, A. C. SARS-CoV-2 threat perception and willingness to vaccinate: The mediating role of conspiracy beliefs. Front. Psychol. 12, 672634. https://doi.org/10.3389/fpsyg.2021.672634 (2021).
MaristPoll. COVID-19 Vaccine Hesitancy, <https://maristpoll.marist.edu/covid-19-vaccine-hesitancy/ (2021).
Olsson, A., Knapska, E. & Lindstrom, B. The neural and computational systems of social learning. Nat. Rev. Neurosci. 21, 197–212. https://doi.org/10.1038/s41583-020-0276-4 (2020).
Franks, B., Bangerter, A. & Bauer, M. W. Conspiracy theories as quasi-religious mentality: An integrated account from cognitive science, social representations theory, and frame theory. Front. Psychol. 4, 424. https://doi.org/10.3389/fpsyg.2013.00424 (2013).
Centola, D. The spread of behavior in an online social network experiment. Science 329, 1194–1197. https://doi.org/10.1126/science.1185231 (2010).
Broniatowski, D. A. & Reyna, V. F. To illuminate and motivate: A fuzzy-trace model of the spread of information online. Comput. Math. Organ Theory 26, 431–464. https://doi.org/10.1007/s10588-019-09297-2 (2020).
van Os, J., Linscott, R. J., Myin-Germeys, I., Delespaul, P. & Krabbendam, L. A systematic review and meta-analysis of the psychosis continuum: Evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol. Med. 39, 179–195. https://doi.org/10.1017/S0033291708003814 (2009).
Peters, E., Joseph, S., Day, S. & Garety, P. Measuring delusional ideation: The 21-item Peters et al. Delusions Inventory (PDI). Schizophr. Bull. 30, 1005–1022 (2004).
Eisenacher, S. & Zink, M. Holding on to false beliefs: The bias against disconfirmatory evidence over the course of psychosis. J. Behav. Ther. Exp. Psychiatry 56, 79–89. https://doi.org/10.1016/j.jbtep.2016.08.015 (2017).
Schmack, K. et al. Delusions and the role of beliefs in perceptual inference. J. Neurosci. 33, 13701–13712. https://doi.org/10.1523/JNEUROSCI.1778-13.2013 (2013).
Schmack, K., Rothkirch, M., Priller, J. & Sterzer, P. Enhanced predictive signalling in schizophrenia. Hum. Brain Mapp. 38, 1767–1779. https://doi.org/10.1002/hbm.23480 (2017).
Teufel, C. et al. Shift toward prior knowledge confers a perceptual advantage in early psychosis and psychosis-prone healthy individuals. Proc. Natl. Acad. Sci. USA 112, 13401–13406. https://doi.org/10.1073/pnas.1503916112 (2015).
Kapur, S. Psychosis as a state of aberrant salience: A framework linking biology, phenomenology, and pharmacology in schizophrenia. Am. J. Psychiatry 160, 13–23. https://doi.org/10.1176/appi.ajp.160.1.13 (2003).
Sterzer, P. et al. The predictive coding account of psychosis. Biol. Psychiatry https://doi.org/10.1016/j.biopsych.2018.05.015 (2018).
Moritz, S. & Woodward, T. S. A generalized bias against disconfirmatory evidence in schizophrenia. Psychiatry Res. 142, 157–165. https://doi.org/10.1016/j.psychres.2005.08.016 (2006).
Woodward, T. S., Moritz, S. & Chen, E. Y. The contribution of a cognitive bias against disconfirmatory evidence (BADE) to delusions: A study in an Asian sample with first episode schizophrenia spectrum disorders. Schizophr. Res. 83, 297–298. https://doi.org/10.1016/j.schres.2006.01.015 (2006).
Woodward, T. S., Moritz, S., Cuttler, C. & Whitman, J. C. The contribution of a cognitive bias against disconfirmatory evidence (BADE) to delusions in schizophrenia. J. Clin. Exp. Neuropsychol. 28, 605–617. https://doi.org/10.1080/13803390590949511 (2006).
Woodward, T. S., Moritz, S., Menon, M. & Klinge, R. Belief inflexibility in schizophrenia. Cogn. Neuroeuropsychiatry 13, 267–277. https://doi.org/10.1080/13546800802099033 (2008).
Riccaboni, R. et al. Patterns of evidence integration in schizophrenia and delusion. Psychiatry Res. 200, 108–114. https://doi.org/10.1016/j.psychres.2012.04.005 (2012).
Eisenacher, S. et al. Bias against disconfirmatory evidence in the “at-risk mental state” and during psychosis. Psychiatry Res. 238, 242–250. https://doi.org/10.1016/j.psychres.2016.02.028 (2016).
Orenes, I., Navarrete, G., Beltran, D. & Santamaria, C. Schizotypal people stick longer to their first choices. Psychiatry Res. 200, 620–628. https://doi.org/10.1016/j.psychres.2012.03.030 (2012).
Buchy, L., Woodward, T. S. & Liotti, M. A cognitive bias against disconfirmatory evidence (BADE) is associated with schizotypy. Schizophr. Res. 90, 334–337. https://doi.org/10.1016/j.schres.2006.11.012 (2007).
Zawadzki, J. A. et al. Cognitive factors associated with subclinical delusional ideation in the general population. Psychiatry Res. 197, 345–349. https://doi.org/10.1016/j.psychres.2012.01.004 (2012).
Woodward, T. S., Buchy, L., Moritz, S. & Liotti, M. A bias against disconfirmatory evidence is associated with delusion proneness in a nonclinical sample. Schizophr. Bull. 33, 1023–1028. https://doi.org/10.1093/schbul/sbm013 (2007).
Kuhn, S. A. K., Lieb, R., Freeman, D., Andreou, C. & Zander-Schellenberg, T. Coronavirus conspiracy beliefs in the German-speaking general population: Endorsement rates and links to reasoning biases and paranoia. Psychol. Med. https://doi.org/10.1017/S0033291721001124 (2021).
Larsen, E. M., Donaldson, K. R., Liew, M. & Mohanty, A. Conspiratorial thinking during COVID-19: The roles of paranoia, delusion-proneness, and intolerance of uncertainty. Front. Psychiatry 12, 698147. https://doi.org/10.3389/fpsyt.2021.698147 (2021).
Louzolo, A. et al. Delusion-proneness displays comorbidity with traits of autistic-spectrum disorders and ADHD. PLoS ONE 12, e0177820. https://doi.org/10.1371/journal.pone.0177820 (2017).
Sanford, N., Veckenstedt, R., Moritz, S., Balzan, R. P. & Woodward, T. S. Impaired integration of disambiguating evidence in delusional schizophrenia patients. Psychol. Med. 44, 2729–2738. https://doi.org/10.1017/S0033291714000397 (2014).
Bronstein, M. V. & Cannon, T. D. Measuring bias against disconfirmatory evidence: An evaluation of BADE task scoring methods and the case for a novel method. Psychiatry Res. 261, 535–540. https://doi.org/10.1016/j.psychres.2018.01.007 (2018).
Peterson, R. A. & Cavanaugh, J. E. Ordered quantile normalization: A semiparametric transformation built for the cross-validation era. J. Appl. Stat. 47, 2312–2327 (2020).
R: The R Project for Statistical Computing (https://www.r-project.org/).
Kessler, R. C. et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): A short screening scale for use in the general population. Psychol. Med. 35, 245–256 (2005).
Ritvo, R. A. et al. The Ritvo Autism Asperger Diagnostic Scale-Revised (RAADS-R): A scale to assist the diagnosis of Autism Spectrum Disorder in adults: An international validation study. J. Autism Dev. Disord. 41, 1076–1089. https://doi.org/10.1007/s10803-010-1133-5 (2011).
Rosseel, Y. lavaan: An R package for structural equation modeling. J. Stat. Softw. 48, 1–36 (2012).
March, E. & Springer, J. Belief in conspiracy theories: The predictive role of schizotypy, Machiavellianism, and primary psychopathy. PLoS ONE 14, e0225964. https://doi.org/10.1371/journal.pone.0225964 (2019).
Swami, V., Weis, L., Lay, A., Barron, D. & Furnham, A. Associations between belief in conspiracy theories and the maladaptive personality traits of the personality inventory for DSM-5. Psychiatry Res. 236, 86–90. https://doi.org/10.1016/j.psychres.2015.12.027 (2016).
Rocchi, M. B. et al. Latent class analysis of delusion-proneness: Exploring the latent structure of the Peters et al. delusions inventory. J. Nerv. Ment. Dis. 196, 620–629. https://doi.org/10.1097/NMD.0b013e31818132a3 (2008).
Bruder, M., Haffke, P., Neave, N., Nouripanah, N. & Imhoff, R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: Conspiracy mentality questionnaire. Front Psychol 4, 225. https://doi.org/10.3389/fpsyg.2013.00225 (2013).
Petrovic, P. & Castellanos, F. X. Top-down dysregulation-from ADHD to emotional instability. Front. Behav. Neurosci. 10, 70. https://doi.org/10.3389/fnbeh.2016.00070 (2016).
Ruzich, E. et al. Measuring autistic traits in the general population: A systematic review of the Autism-Spectrum Quotient (AQ) in a nonclinical population sample of 6,900 typical adult males and females. Mol. Autism 6, 2. https://doi.org/10.1186/2040-2392-6-2 (2015).
Franks, B., Bangerter, A., Bauer, M. W., Hall, M. & Noort, M. C. Beyond, “Monologicality”? Exploring conspiracist worldviews. Front. Psychol. 8, 861. https://doi.org/10.3389/fpsyg.2017.00861 (2017).
Mohr, C. & Claridge, G. Schizotypy–do not worry, it is not all worrisome. Schizophr. Bull. 41(Suppl 2), S436-443. https://doi.org/10.1093/schbul/sbu185 (2015).
Javitt, D. C. & Freedman, R. Sensory processing dysfunction in the personal experience and neuronal machinery of schizophrenia. Am. J. Psychiatry 172, 17–31. https://doi.org/10.1176/appi.ajp.2014.13121691 (2015).
Sterzer, P., Frith, C. & Petrovic, P. Believing is seeing: Expectations alter visual awareness. Curr. Biol. 18, R697. https://doi.org/10.1016/j.cub.2008.06.021 (2008).
Kappes, A., Harvey, A. H., Lohrenz, T., Montague, P. R. & Sharot, T. Confirmation bias in the utilization of others’ opinion strength. Nat Neurosci 23, 130–137. https://doi.org/10.1038/s41593-019-0549-2 (2020).
Nickerson, R. S. Confirmation bias: A ubiquitous phenomenon in many guises. Rev. Gen. Psychol. 2, 175–220 (1998).
Balzan, R., Delfabbro, P., Galletly, C. & Woodward, T. Confirmation biases across the psychosis continuum: The contribution of hypersalient evidence-hypothesis matches. Br. J. Clin. Psychol. 52, 53–69. https://doi.org/10.1111/bjc.12000 (2013).
Sharot, T. & Sunstein, C. R. How people decide what they want to know. Nat. Hum. Behav. 4, 14–19. https://doi.org/10.1038/s41562-019-0793-1 (2020).
Jung, H. Y. et al. Measuring psychosis proneness in a nonclinical Korean population: Is the Peters et al Delusions Inventory useful for assessing high-risk individuals?. Compr. Psychiatry 49, 202–210. https://doi.org/10.1016/j.comppsych.2007.08.011 (2008).
Chan, C. C. et al. Comparison of self-report and clinician-rated schizotypal traits in schizotypal personality disorder and community controls. Schizophr. Res. 209, 263–268. https://doi.org/10.1016/j.schres.2018.12.050 (2019).
Dagnall, N., Drinkwater, K., Parker, A., Denovan, A. & Parton, M. Conspiracy theory and cognitive style: A worldview. Front. Psychol. 6, 206. https://doi.org/10.3389/fpsyg.2015.00206 (2015).
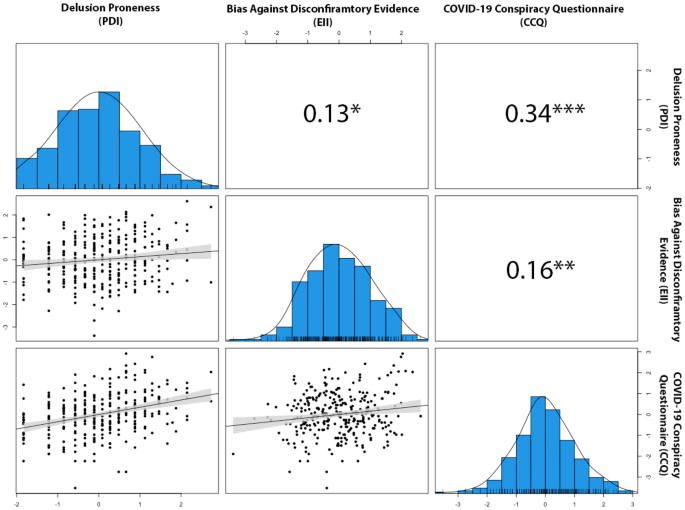
Georgiou, N., Delfabbro, P. & Balzan, R. Conspiracy-beliefs and receptivity to disconfirmatory information: A study using the BADE task. SAGE Open 11, 1–9 (2021).


