newsGP – Migrants more than twice as likely to die of COVID-19
News
The burden of the pandemic hugely and disproportionately lies among those born overseas, official ABS figures show.
Gaping inequities in the impact of COVID-19 have been laid bare in recent figures released by the Australian Bureau of Statistics (ABS).
Those born overseas are more than twice as likely to die from the disease as people born in Australia, ABS mortality figures up until June this year suggest.
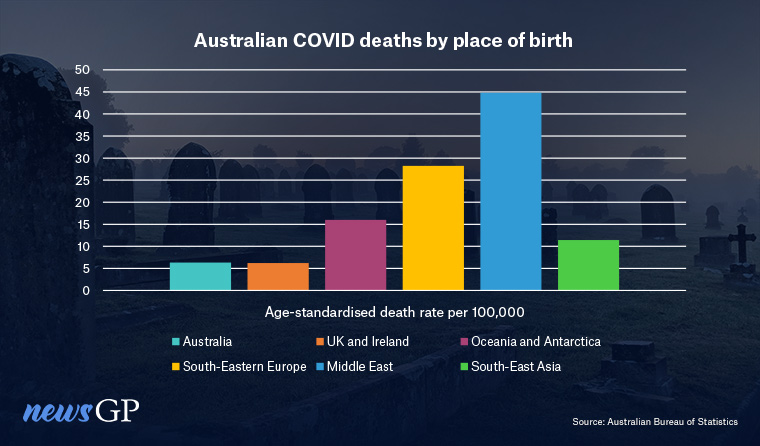
Those born in the Middle East have by far the highest age-standardised death rate, with the ABS reporting 44.8 deaths per 100,000 among residents born in countries from that region – more than seven times the rate for people of Australian birth.
While the impact is greater overall among those born overseas, the burden is unevenly spread. The ABS reports, for example, that those born in the United Kingdom and Ireland had a lower age-standardised death rate of 6.2 per 100,000 people than the Australian-born average of 6.3.
The total number of deaths also tell a similar story.
For the period covered by the ABS, there were 2577 Australian-born people dying from COVID-19 recorded until 31 May compared to 3525 among those whose birthplace is outside Australia, a difference of 37%. The latest census puts just over a quarter of Australians (27.6%) as born outside the country.
The ABS makes no link between the death rate and vaccinations, but the association is clearly being made elsewhere. Associate Professor Michael Murray, a geriatrician and president of President of the National Ageing Research Institute, recently told Nine Newspapers that vaccination in Culturally and Linguistically Diverse (CALD) groups such as the Greek community is ‘depressingly low’.
The ABS figures show 1525 deaths attributed to COVID-19 so far among people from southern and south-Eastern Europe, a figure likely to have risen significantly in the past month.
Melbourne GP Dr Magdalena Simonis has been a constant advocate for vaccine uptake in the Greek community, including helping with vaccinations offered through a Greek Orthodox Church last year.
However, she reports repeated issues in convincing patients to be up to date with their COVID-19 immunisations.
‘We’ve had a great deal of trouble getting the elderly to agree to have three injections,’ she told newsGP.
‘And having the fourth injection has been even more challenging. We know that with the vulnerable and the elderly the fourth actually does make a huge difference.’
Dr Simonis says there is also significant hesitancy with the flu vaccine and believes campaigns for the more recent COVID-19 rollout have not been targeted at different cultural groups with enough accuracy.
‘We’ve found that a lot of the communication and a lot of the messaging is not culturally specific,’ she said.
‘Every culture has its own idiosyncrasies and ways of describing things. We know all our different cultural groups have different ways of interpreting the information that they receive.
‘It really does require targeted, culture-specific health promotion that engages primary care physicians, doctors like myself, with the creation of the messaging based upon the obstacles that we’ve observed and the conversations that we are facing.’
She hopes the ABS data will be used to help sway more government support for tailored messages that involve primary care.
‘We are still the trusted source of health information,’ Dr Simonis said.
‘It’s not so much government websites, it is still the GP that works within the community who has even more of that gravitas and trust.’
Data gaps
Associate Professor Margie Danchin, who sits on the Collaboration on Social Science and Immunisation (COSSI), described the ABS figures as ‘shocking’ and ‘very upsetting’.
She believes the gap in evidence surrounding CALD communities and the higher mortality rate urgently needs to be addressed.
‘Being able to look at vaccine coverage by different communities and different demographic variables, including age, ethnicity, and other comorbidities, or other conditions like pregnancy, our data is terrible,’ she told newsGP.
‘We just cannot get this granularity to be able to truly understand.’
Associate Professor Danchin says she has encountered CALD communities where there are strongly held beliefs in conspiracy theories, which she says are stalling booster uptake. Like Associate Professor Simonis, she believes the solution lies in breathing new life into approaches tailored to different sections of the population – a tactic she says worked well in the initial phase of the vaccine rollout.
‘Why are we spending $11 million on another faceless “Arm Yourself” campaign to promote boosters that’s not going to really change people’s minds?’ she said.
‘Why are we not putting that funding into grassroots community engagement campaigns?’
Associate Professor James Wood, an applied mathematician from the UNSW’s School of Population Health, has drawn attention to the ABS figures on social media.
He says that ‘siloed’ data – with vaccination figures separate to details on cases and mortality – has led to insufficient publicly available information on the differences in serious outcomes. However, he is hopeful that a new data integration project known as AIR-MADIP will address that issue.
Associate Professor Wood also makes the point that the uneven impact of COVID previously reflected the greater risk of infection in poorer areas with larger migrant populations, where people often work in roles that cannot be done from home.
Now he thinks there are different dynamics at play.
While the risk of infection is more evenly spread, like Associate Professor Murray links the severity of disease in part to variations in booster coverage.
‘Post mandates, we’re seeing big gaps in vaccine uptake,’ he told newsGP.
‘This reflects multiple factors but education, language, and increased hesitancy due to anti-vaccine messaging in non-English languages are all in the mix.
‘The end outcome is higher risk of hospitalisation and death in migrant communities.’
Log in below to join the conversation.

