COVID-19 Jab Does Not Work. Here’s Why
A team of Harvard research scientists, publishing in the New England Journal of Medicine, have found that SARS-CoV-2 virus has mutated so much that the Pfizer mRNA vaccines developed against the original Wuhan strain now have little to no effect.
The study, “Neutralization Escape by SARS-CoV-2 Omicron Subvariants BA.2.12.1, BA.4, and BA.5,” evaluated neutralizing antibody titers of participants vaccinated with the Pfizer vaccine, against multiple SARS-CoV-2 strains.
The scientists found that the titers dropped from 5,783 (against the WA1/2020 isolate, Wuhan strain) to 275 (against the BA.4 or BA.5 subvariant, omicron variants), by a factor of 21.
In other words, they found the mRNA vaccine to be essentially ineffective against Omicron variants currently in circulation.
SARS-CoV-2 Mutations
SARS-CoV-2 has been a quickly evolving virus since late 2019. Like all RNA viruses, it has a strand of RNA that is packaged in a delivery vehicle that allows it to attach itself to host cells and inject its RNA into the cells and hijack the cells to make more copies of its RNA.
A virus must interact with living cells in order to reproduce. Without this interaction, the virus itself is inert. It has no metabolism. It cannot move. It doesn’t eat. It cannot reproduce with other viruses. What this means is that a virus has none of the characteristics of living organisms. Because of this, some scientists want to classify viruses as part of life while others point out that viruses are not alive. At least not without hosts.
Life or not, all viruses must have genetic material RNA (ribonucleic acid) or DNA (deoxyribonucleic acid). RNA or DNA make copies using templates of complementary strands of RNA or DNA. There is always a chance for errors to happen during this process. We call these “errors” mutations.
Often these errors make the DNA or RNA too imperfect to carry on functioning, so the mutation goes nowhere. But if the mutated version is viable, the result is a new, slightly changed version of the DNA or RNA.
A virus that does not kill its host but is able to keep using the host to replicate itself is able to continue replicating. There is an advantage to a virus developing a way to become chronic or endemic, rather than being rabidly lethal to the host.
By every indication, that is what is happening with SARS-CoV-2, the novel virus that likely originated in Wuhan, China, and quickly spread around the globe, using humans and other animals as its host.
Anti-Spike Antibodies
Many of the mutations to the SARS-CoV-2 RNA do not change any of the proteins the virus needs to survive and proliferate. These are called silent or synonymous mutations. Others, known to scientists as non-synonymous mutations, do change the amino acid composition of the proteins.
The amino acid sequence differences (about 3 percent) observed between SARS-CoV-2 spike proteins from the original Wuhan strain (GenBank # YP_009724390) and an Omicron isolate from Norway on January 3rd, 2022 (GenBank # UOU35996.1) are the results of two years of evolution of the virus on its spike protein.
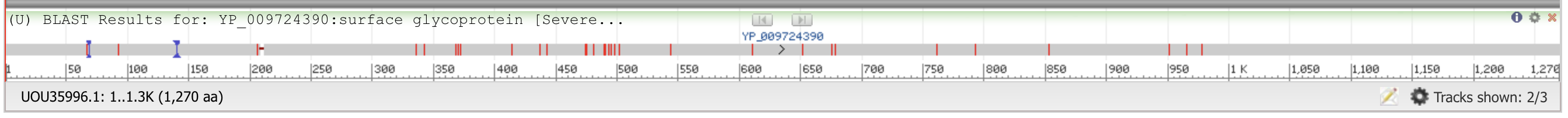
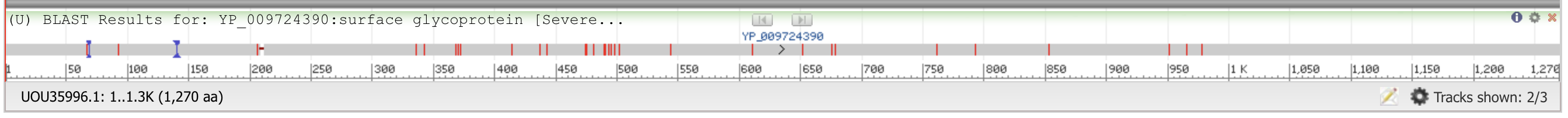 (National Library of Medicine’s online Blast service)
(National Library of Medicine’s online Blast service)Using the National Library of Medicine’s online Blast service, the authors compared the spike protein sequences from the Wuhan strain and an Omicron variant. The red lines highlight the mismatches.
Compared to other parts of the virus genome, the gene that codes for the spike protein evolve faster, as the spike protein is on the surface of the virus and is under much more selection pressure.
This poses a problem for the current vaccines and any future vaccines based on the spike protein. The fast-changing spike protein would likely make the existing vaccines and any new vaccines less effective. In other words, the virus has moved on, but the vaccines have not.
Existing vaccines based on the spike protein generate multiclonal antibodies against different epitopes of the spike protein. If an antibody reacts to an epitope that is not affected by the mutations that Omicron has, then this antibody would be effective against Omicron. Otherwise, it will not be effective.
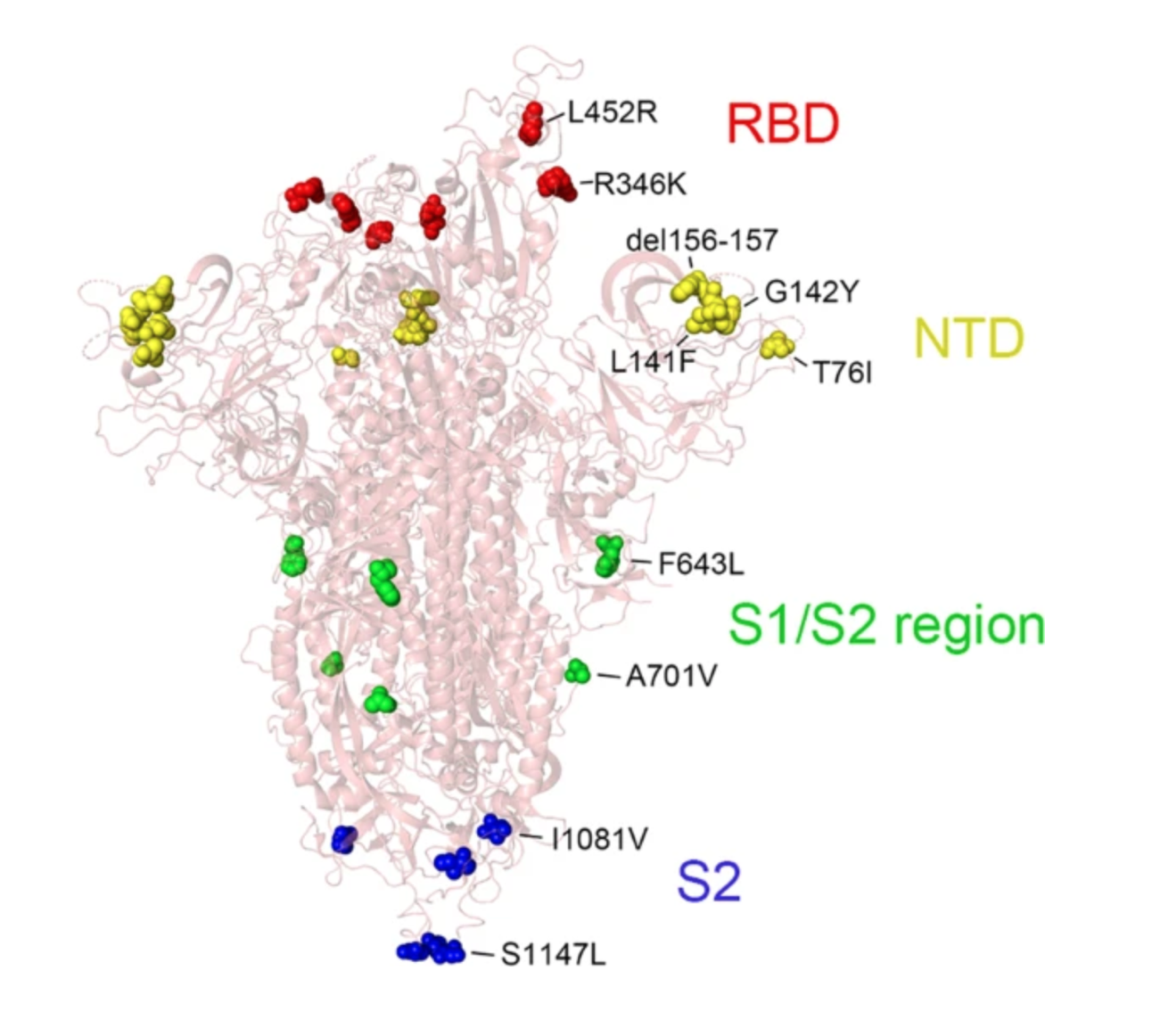
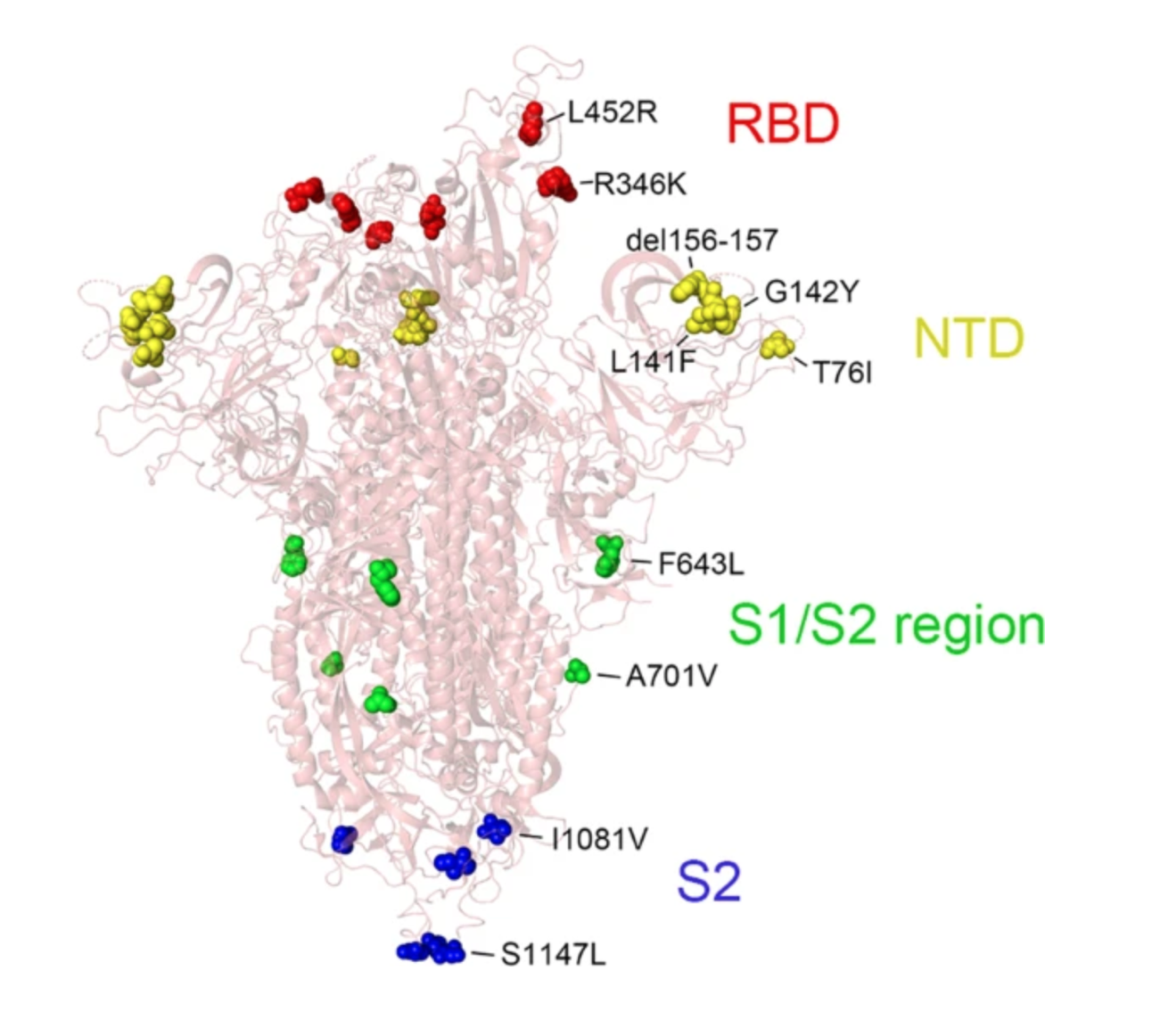 Structure of SARS-CoV-2 Omicron spike protein mapped with the novel mutations. (Source: Tracking SARS-CoV-2 Omicron diverse spike gene mutations identifies multiple inter-variant recombination events)
Structure of SARS-CoV-2 Omicron spike protein mapped with the novel mutations. (Source: Tracking SARS-CoV-2 Omicron diverse spike gene mutations identifies multiple inter-variant recombination events)When most, if not all antibodies that the COVID-19 mRNA vaccines developed based on the original Wuhan strain fails to react to the current SARS-CoV-2 variant, the vaccine becomes ineffective.
Vaccinated Have Negligible Antibodies Against Current Strain
In the new Harvard study, the scientists tested 27 participants who had been vaccinated with Pfizer’s messenger RNA vaccine (BNT162b2) and 27 participants who had been infected naturally with the original Wuhan strain.
Most of those who had had COVID already had also been vaccinated, so most, but not all, had hybrid immunity.
Those who had recovered from COVID had a strong immune response to the original virus, which is no longer circulating in the world.
But those who had been vaccinated just six months prior to the test had only 1 percent as many antibodies as those who had recovered from having the virus.
Participants who had been boosted just two weeks before the test and were at the peak of their immunity did have a strong response, though it was still half as strong as those with natural immunity. Evidently their vaccine-acquired immune response was not long lasting, either.
And these results were only for the original, outdated virus, which is no longer a danger.
Against the strain currently dominant in the United States, those who had been vaccinated, even at the peak of their protection two weeks after the booster, had a very scant antibody response to the current virus, about 7 percent as strong as their antibody response to the original 2020 virus.
Those who were vaccinated six months before, but not boosted, had negligible antibodies against the current virus.
Natural Immunity Provides Substantial Immune Response
Those with natural immunity after recovering from COVID had a substantial immune response to the current virus.
Though it was only 10 percent as strong as their response to the original 2020 virus, their immune systems still responded with three times as many antibodies as the boosted group’s peak response.
More importantly, compared to immunity acquired through the spike-protein-based vaccines, natural immunity from SARS-CoV-2 infections covers the whole spectrum of immunity, giving the body short-term antibody protection as well as memory B and T cells for long-term protection. In addition, the short-term antibodies cover not only the fast-changing spike protein (S), but also other viral proteins, such as nucleocapsid protein (N) and envelope protein (E), making natural immunity less vulnerable for immune escape.
The takeaway is that even for the brief period right after a booster, vaccination was not as effective as natural immunity. Six months later, it was essentially useless.
The good news is that almost everyone in the U.K. has SARS-CoV-2 antibodies. This suggests that almost everyone there has had a SARS-CoV-2 infection at some point, and so has some level of natural immunity.
This does not mean that COVID-19 is over. It does mean that nature has provided people in the U.K. with protection better than the current spike-protein-based vaccines.
We believe that the same is true in the United States and Canada.
Take the jab, if you want, and get the boosters. But don’t be fooled. They will not give you any more protection than what you already have.
Views expressed in this article are the opinions of the author and do not necessarily reflect the views of The Epoch Times. Epoch Health welcomes professional discussion and friendly debate. To submit an opinion piece, please follow these guidelines and submit through our form here.
This article has been archived for your research. The original version from Epoch Times can be found here.


