Covid-19 on Pharmaceuticals Shortages And Supply Disruptions | JMDH
Introduction
Due to the current critical situation, it seems necessary to design an appropriate medicine supply chain network that can provide appropriate medicines to COVID-19 patients in an organized manner. Therefore, inventory control and management of medicine distribution in such conditions due to the perishability of medicines can reduce human casualties and increase the health of patients. In addition, uncertainty in the supply chain network of medicine distribution is an integral part. The demand in hospitals for various medicines is scattered and should always be seen as unpredictable. For this reason, the sensitivity of work in completing this supply chain increases.1 Also, reports from European Commission indicated that currently the Covid 19 pandemic has led to inequitable supply and shortages of essential medicines worldwide due to decreased production capacity, export bans, and national stockpiling which are affecting the global pharmaceutical supply chain.2 Pharmaceuticals are an integral part of healthcare delivery, which play a great role in improving treatment outcome and quality of healthcare service.3 Availability of essential medicines at public health facilities is less than 60% across WHO regions, especially in African region.4 The longstanding pharmaceutical shortage has worsened due to the ongoing pandemic of Covid 19 which has disrupted production of essential medicines, medical supplies as well as raw materials, and has a potential to put an increasing strain on the global pharmaceutical supply.5 According to epidemiologists and the researchers’ results, the only way to definitively break the coronavirus chain is through general vaccination, and means such as global quarantine or the use of masks offer only temporary protection.6 Moreover, it is necessary to design a supply chain network (SCN) that can monitor the inventory of medicines and can control the flow between members of the supply chain. The location of distribution centers and warehouses in this chain also accelerates the distribution of medicines and minimizes total costs.7
According to WHO’s rapid assessment among 163 Ministries of Health, the more severe the transmission phase of the COVID-19 pandemic, the more non-communicable disease (NCD) services such as Hypertension Management, Diabetes and Diabetic Complications Management, Asthma services, Cancer Treatment and Cardiovascular emergencies were disrupted as of May 2020. A study from different scholars showed that among 122 countries of the world, 20% reported the main causes of NCD services disruption in healthcare facilities was unavailability/out of stock essential medicines, medical diagnostics and health products.8 Thus it is crucial to assess the impact of Covid-19 pandemic on pharmaceutical shortages and supply disruptions for non-communicable diseases at public hospitals of Ilu-Abba-Bor and Bunno-Beddele Zones, Oromia, Ethiopia during the era of Covid-19 pandemic since no study has been done in the remote zone of Oromia, which is the study area of this research.
Methodology and Materials
Study Setting and Period
This study was conducted in selected public facilities and quarantine centers in Ilu Abba Bor and Buno Bedelle Zones, Oromia Regional state, south-west of Ethiopia. Ilu Abba Bor zone and Buno Bedelle Zone are from the 20 zones of Oromia regional state situated south-west of the region and located at a distance of about 600 km and 483 from the center of the region respectively. In the two zones there are six functional hospitals namely: Bedele hospital, Darimu hospital, Chawaka hospital, Metu Karl hospital, Dedhesa hospital and Cora hospital. The pharmaceuticals required for service provisions in all public health facilities found in these two zones are supplied mainly from Ethiopian Pharmaceuticals Supply Agency (EPSA)/Jimma Hub. EPSA is the semi-autonomous governmental organization which is responsible for planning and implementing the national essential pharmaceutical supply system in public health facilities of Ethiopia. The study was conducted from March 1–30, 2021.
Study Design
A multi-institutional-based descriptive cross sectional study design was used in which both quantitative and qualitative methods were employed concurrently. The data that were collected from health facilities, patients, and local health authorities were employed to characterize and assess the pharmaceutical supply disruption and shortages in the study area.
Population
Source population
All pharmaceuticals used, all health professionals, all patients visiting pharmacy services and all prescriptions dispensed in public hospitals, and all personnel working in local health authorities in both Ilu Ababor and Buno Bedelle zones were source population/data.
Study Population
All essential pharmaceuticals (medicines and laboratory reagents) approved in formulary for NCD management, all drug and therapeutic committee (DTC) members, all patients visiting pharmacy services and all dispensed prescriptions with medicines for NCD in selected public hospitals and all focal personnel from local health authorities working in both Ilu Abba-bor and Bunno-Bedelle zones were study population.
Inclusion and Exclusion Criteria
Inclusion
Vital pharmaceuticals from revolving drug fund (RDF) used in NCD management, key informants from drug and therapeutic committee members, patients visiting pharmacy services on the days of visit at public hospitals and focal personnel working in hospital or pharmaceuticals management related position in both Ilu Aba-Abor and Bunno-Bedelle zones were included in the study.
Exclusion
Public hospitals with less than one year of service and with weak pharmaceutical services, all program pharmaceuticals, all personnel who are not directly involved in pharmaceutical management activities and all patients less than 18 years of age were excluded from the study.
Sample Size and Sampling Techniques
The sample size of the public hospitals were determined by considering at least 15% of the total public hospitals and 100 prescriptions per hospital was selected by simple random sampling method based on the USAID delivery project logistics indicators assessment tool.9,10 Accordingly samples were selected from four public hospitals (Beddele Hospital, Didesa Hospitals, Mettu Karl Specialized Hospital and Darimu Hospital) by stratified simple random sampling from each zone. Considering the top ten diseases of the study area and after consulting the standard treatment guidelines, selected first line essential pharmaceuticals used in the management of NCDs among selected public hospitals were used as essential tracer pharmaceuticals to assess the availability status. The sampling procedure for patient interviews and key informant interviews was based on the saturation of ideas for qualitative information.
Study Variables
Dependent Variable
Availability of pharmaceuticals and pharmaceutical supply disruption.
Independent Variables
Impact of covid-19 pandemic disease, financial resource/funding, inventory management, human resources, capacity development, supplier uncertainty/performance, work load/patient flow, supportive supervision and monitoring and evaluation.
Data Collection Methods and Tools
Standardized observational check-list and semi-structured interview adopted from WHO and USAID Deliver Project logistic indicators assessment tools and Ethiopian Food, Health and Drug Administration guidelines were used to collect quantitative data related to availability of pharmaceuticals, and the qualitative data were collected through conducting interviews with key informants from local health authorities and DTC chief members by using interview guide with flexible probing.
Data Processing and Analysis
After data collection was completed, each observation checklist was checked for completeness, missing values and unlikely responses and then manually cleaned. Then the cleaned data were coded and entered into Microsoft Excel and then exported to SPSS (version 23.0). The audio recorded and written notes were transcribed verbatim, coded, and analyzed by all authors. The qualitative data collected through in-depth interview were analyzed through thematic approach and summarized in narrative form.
Operational Definitions
Pharmaceuticals: essential medicines, critical medical supplies and laboratory reagents required for management of non-communicable diseases (NCD) such as hypertension, diabetes mellitus, asthmatic disorders and epilepsy management in public hospitals of the study area.
Pharmaceutical supply disruptions: defined as discontinuations of pharmaceutical product lines from suppliers to public hospitals and causing out of stock pharmaceuticals at the point of use for the purpose of this study.
Pharmaceutical shortage: defined as a situation in which the total supplies of approved pharmaceuticals are inadequate to meet the current demand and requiring a change since it impacts patient care at the hospital level for the purpose of this study.
Revolving Drug Fund Pharmaceuticals: defined as medicines, medical supplies and laboratory reagents that were procured through hospitals’ treasury budget and it excluded all program pharmaceuticals obtained through donation for this study.
Result
Socio-Demographic Characteristics of the Key Informants
Among the 20 respondents, 15 (75%) were male. The majority (10 [50%]) of them were in the age group between 20–30 years old. Regarding their profession, majority of the respondents were pharmacy staff (12 [60%]) followed by physicians (4 [20%]). Regarding role in pharmaceutical management, majority 7(35%) of them were facility medical storeman. In addition, 10 (50%) of the respondents had between 5–10 years of professional work experience and socio-demographic characteristics of the key informants can be seen in Table 1.
 |
Table 1 Sociodemographic Characteristics of Key Informants Working in the Selected Public Hospitals of Illu Aba Bor and Buno Bedelle Zone, Ethiopia, May 2021 (n = 20) |
Extracted Information from Key Informants of Selected Public Hospitals of Illu Aba Bor and Buno Bedelle Zone
Key informants reported shortage at supplier and public health facilities related factors as reasons for essential medicine wastage for non-communicable disease during COVID-19 pandemic disease (Table 2). A statement made by one key informant demonstrated this fact:
Essential medicine wastage in our facility during era of Covid-19 pandemic disease is a result of internal factor like shortage of pharmacy professional and lack of administrative support) and external factors (e.g. Supplier challenges). (CEO of facility)
Our supplier does not usually provide us the medicines as per the requested type and quantity. For example, we recently received several tins of prednisolone that we had not ordered because we have ordered essential medicine used for treatment of non-communicable disease since in our hospital most of the patient has been admitted were from non-communicable disease. Most of the time they do this to balance/match the budget we have with the value (financial) of products they issue. They themselves adjust the quantity and provide us overstock medicines which mean imbalance between demand and supply …. such practice led to essential medicines shortage for non-communicable diseases. (Facility pharmacy Head)
 |
Table 2 Main Themes/Categories and Sub-Themes Extracted from Key Informants of Selected Public Hospitals of Illu Aba Bor and Buno Bedelle Zone, South West, Ethiopia, May 2021 |
Budget. The inadequacy of budget was mentioned by key informants (KIs) as a significant challenge for shortage of essential medicine for non-communicable diseases during covid-19 pandemic disease in public hospital of Buno Bedelle and Ilu abba bor Zone. Some of the KIs mentioned that “they try to give priority for the procurement of NCD products in case of budget shortage”.
Proposed Solutions for Pharmaceutical Shortage for Non-Communicable Diseases During Era of Covid-19 Pandemic in Public Hospitals
One Participant mentioned that
Additional budget allocation for life saving medicine for NCD, exchange of physical stock with other near health facilities like from Jimma health facility, optimize utilization and consider for alternative private suppliers is proposed solutions for pharmaceuticals shortage in public hospitals during the era covid-19 pandemic disease. (DTC members)
The Effect of Covid-19 on Essential Medicine Used for Non-Communicable Diseases During Era of Covid-19 Pandemic Disease
Regarding the cost effect of COVID-19 on essential medicine used for non-communicable diseasis in public hospitals of Illu aba bor and buno Bedele Zone, cost of medicine increased more in Dedesa hospital compared to other public hospital both found in zone and the effect of Covid-19 on essential medicine used for treatment of non-communicable diseases was less in the case of Darimu Hospital. The assessment of effects of Covid-19 on essential medicine used for treatment of non-communicable diseases is shown in Figure 1.
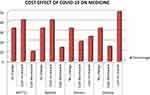 |
Figure 1 The effect of Covid-19 on cost of essential medicine used for NCD in selected hospitals of Illu aba bor and Buno bedelle Zone, South west Ethiopia. |
Total Number of Days for Out of Stock and Dispensed Medicine in Most Recent 6 Months During Era of Covid-19 Pandemic Disease
The most dispensed medicines obtained from public hospitals were primarily from hypertension (40%) and diabetes drugs (35%) and based on the duration of therapeutic regimen, majority of the drugs that were out of stock in selected hospitals of Illu aba bor and Buno bedelle Zone, South west of Ethiopia were those agents being used for treatment of hypertension and the highest rate of out of stock medicine was in Mettu Karl hospital compared to other public hospitals in both zones. The total numbers of days for out of stock and dispensed medicine in most recent 6 months were shown in Figure 2.
 |
Figure 2 Total number of days out of stock of drugs used for treatment of NCD in selected hospitals of Illu abba bor and Bunno bedelle Zone, South west Ethiopia. |
The Names of Out of Stock Medicines and Strength for Treatment of NCD from Patient Interview During Era of Covid-19 Pandemic Disease
Of the 24 essential medicines, 14 were available in all public hospitals at the day of visit while Isophane insulin human 100Iu/mL, was out of stock on day of visit and in the last 6 months in all PHs. Interview with patients on the day of hospital visit revealed that, the most frequently out of stock medicine in the public hospitals of both zones were Enalapril Maleate 10mg, Hydrochlorothiazide 25mg, Nifedipine 20 mg and Metformin 500 mg, as shown in Table 3.
 |
Table 3 The Name of Out of Stock Medicine and Strength for Treatment of NCD in Selected Public Hospitals of Illu Abba Bor and Buno Bedelle Zone from Patient Interviews, South West Ethiopia |
Average Length of Out of Stock for Essential Medicine Used for Non-Communicable Diseases Within the Past 6 Months at Selected Hospitals of Illu Abba Bor and Bunno Bedelle Zone, South West Ethiopia by Interving Storeman Using Standard Check-list
Among four public hospitals, insulin isophane human was out of stock for a longer period of time (93 days) whereas Hydralazine 20 mg was out of stock for shorter duration (5 days) (Figure 3). Among the out of stock drugs, 10 (40.8%) were out of stock in the last six months, for less than 40 days. Drugs which were out of stock for a total of 40–80 days in the last six month period were 12 (16.7%) and two drugs were out of stock for a total of greater than 90 days, as shown in Figure 3.
Discussion
Non-communicable diseases currently need special attention in control and prevention due to the spread of the Covid-19 pandemic disease which is a highly contagious, global pandemic currently affecting people of all ages and sectors without any discrimination.11,12 Thus, the study aimed to evaluate the effect of Covid-19 pandemic on availability of essential medicine for non-communicable diseases and disruption of supply among public hospitals of illu Ababor and buno bedelle zone. In the current study, out of the total invited health professionals and key informants, only 75% were interested in being involved in the study. This may be due to workload because of high cases of Covid-19, fear of COVID-19 transmission, and/or other personal reasons (such as; fear of being exposed as some health professionals were irrationally increasing the price of some pharmaceutical products, mainly for non-communicable diseases). It is vital to mention that the disruption in the availability of essential medicines may overburden the health‑care system during the existing COVID‑19 pandemic and could lead to a doubling in the mortality rates.13 As depicted in Table 2, the reasons for the shortage of essential medicines used for treatment of NCD in public hospitals of illu-abba bor and buno bedelle zone may be multifactorial. There are imbalances in demand versus supply rate, inadequate infrastructure to manage the emergency supply chain, and finally, budget deficit; all these problems are more severe in the resource‑poor setting of low‑ and middle‑income countries like Ethiopia (Table 2).14,15 The approach to mitigating, or the possible solution to decrease the pharmaceutical shortage for non-communicable diseases is by effective communication with nearby public hospitals like from Jimma hospitals about the shortages, and allocating sufficient budget for purchasing essential medicines for non-communicable diseases was stated by one of the key informants. In addition to that, a qualitative part of this study showed that challenges faced during the COVID-19 outbreak helped to further understand the problem from the health professionals that have been working in the public hospitals of both zones, besides, the key informants like CEO of hospital, storeman and DTC members have raised a lot of problems prominently hindering their service delivery practices, specifically patient utilization of essential medicines for NCD. Some examples of these problems were; supply disruption, pre-existing poor infrastructure which increases high rate of bed occupancy, low service utilization of patients due to extended date of follow-up, increased workload of staff because of high cases of Covid-19, increased risk of health professionals getting the virus, and poor job satisfaction of health professionals due to fear of covid-19 outbreak.9,16,17 In addition to that, poor infrastructure such as lack of enough bedrooms and medical equipment may also worsen poor availability of essential medications, staff work overload due to few pharmacy professionals, increased risk of acquiring the infection, and poor patient satisfaction regarding service provided by the facility due to shortage of pharmaceuticals for their disease as stated in CEO interview. The fact that the outbreak occurred mid financial year along with an exhausted and limited budget for some programs might have exacerbated the situation. In fact, within the limit of efforts undertaken so far, the facilities have been shown to collaborate with near facilities like Jimma hospitals, and more allocation of budget for non- communicable diseases was another suggestion as a possible solution to enhance the availability of these pharmaceuticals mentioned by DTC members. In line with this, the patient interviews also mentioned that the implementation of “stay home rules for COVID- 19 suspects” has had a negative influence on old-age patients with comorbid conditions as there is inadequate staff, facilities. More than half of the study participants were requesting direct purchases, also indicating poor medication stock management for emergency drugs like fluid, such as in the COVID-19 pandemic or any disruption of essential drug supply chains.18 The differences in the increases in prices of essential medicines were also varied among public hospitals of two zones and medication price increment due to covid-19 outbreak could be attributed to differences in treatment strategies implemented in each public hospital in the two zones due to the rapidly changing recommendations and new potential therapies.19 Essential medicine price increases were reported by over half of the respondents and the cause of this discrepancy among the respondents is unknown and requires further investigation. Covid-19 pandemic affects availability of essential medicines for non-communicable disease treatment and significantly influences quality of healthcare and patient satisfaction, and out of stock EMs force patients to use more costly alternatives from private drug stores. Drug availability is affected by efficiency of inventory management20 and the overall availability of EMs in this study was far from WHO recommended target point.21 In 2019, the general availability of essential medicine in Ethiopia was reported to be 91% but, studies conducted in different parts of Ethiopia after 2019 showed big variation in the availability of essential medicine ranging from 26 to 91%.22,23 The availability of essential medicine documented in this study is better than in Amhara region but lower compared to Gondar and Addis Ababa.4,24 This might be due to the stock status of regional PFSA and the fact that budgets put on primary public health facilities vary from one region to the other in Ethiopia. The absence of or lack of enough pharmacy professionals is one of the challenges in inventory management practice in the public hospitals in the two zones which further decreases the availability of essential medicine for non-communicable diseases in the public health facilities during the era of covid−19 outbreak.20 The severity of out of stock duration of essential medicine in each public hospital was assessed by calculating the average out of stock days of TDs within the past 6 months. The six month average out of stock days of TDs in this study is lower when compared to the situation in Uganda, 72.9 days, and higher when compared to the result in Gondar, 30.5 days.25 The reason for long out of stock period in this study might be due to transportation because of national lockdown during procurement process and unavailability of the TDs at PFSA, as most professionals stated. Of the 24 TDs, cardiac medicine was out of stock for longer period during covid-19 pandemic disease in the study area when compared to the other TDs used in Gondar, from 26 TDs chloroquine syrup was out of stock for more days.22 The long out of stock period for cardiac medicine like enalapril might be due to its high consumption since it is an important lifesaving medicine for many cardiac diseases, which is common in developing countries like Ethiopia.26 In the present study, drugs for chronic diseases were the most frequently reported group of medications in short supply for public hospitals of the two zones. This finding was in line with a study by Tuccori et al (2020) which reported that the drug demand was increased by 30–40% and related to the COVID-19 outbreak.27 This may be due to the high consumption of those medications by patients due to the stress induced by the pandemic or due to panic-buying and storing due to fear of future shortage of supply.
Conclusion
The availability of essential medicine used for treatment of non-communicable diseases and accurate record-keeping in the public hospitals during the era of Covid-19 pandemic disease in illu abba bor and buno bedelle zones were low. The major problem common for all public hospitals in the procurement process were PFSA stock status and transportation due to covid-19 pandemic disease which causes international lockdown. The lack of enough pharmacy professionals is one of the challenges of proper inventory management practice in the public hospitals, which further decreases the availability of essential medicine for treatment of non-communicable diseases in the facilities.
Abbreviations
COVID-19, Corona Virus Disease 2019; DTC, Drug and Therapeutic Committee; PFSA, Pharmaceuticals Fund Supply Agency; TD, tracer drugs; EM, essential medicines; NCD, non-communicable disease; EPSA, Ethiopian Pharmaceuticals Supply Agency; RDF, Revolving Drug Fund; USAID, United State agency institutional development; CEO, chief executive office; PH, public hospitals; WHO, World Health Organization.
Data Sharing Statement
The datasets (audio records of the key informants and written transcripts) generated and analyzed during the current study are not publicly available because they are confidential in order to protect the participants anonymity.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Institutional Review Board (IRB) of Mattu University and confidentiality during all phases of research activities was kept and data were held on a secure password-protected system. This study was conducted in accordance with the Declaration of Helsinki and the study participants gave their consent for the publication of identifiable details within the text (“Material”) to be published and they confirmed that they have seen and been given the opportunity to read both the material and the article to be published. They have discussed, with an author of this paper, and they also understand that the published materials may be available in both print and on the internet, and will be available to a broader audience through marketing channels and other third parties.
Acknowledgments
We thank Mattu University for logistic support. We are grateful to staff members and healthcare professionals of Metu Karl, Bedele, Dedesa and Darimu hospital, data collectors, and study participants for their cooperation and success of this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was sponsored by Mattu University.
Disclosure
The authors report no conflicts of interest in relation to this work. There are no conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. Goodarzian F, Taleizadeh AA, Ghasemi P, Abraham A. An integrated sustainable medical supply chain network during COVID-19. Eng Appl Artif Intell. 2021;100:104188. doi:10.1016/j.engappai.2021.104188
2. Romano S, Galante H, Figueira D, Mendes Z, Rodrigues AT. Time-trend analysis of medicine sales and shortages during COVID-19 outbreak: data from community pharmacies. Res Social Adm Pharm. 2021;17(1):1876–1881. doi:10.1016/j.sapharm.2020.05.024
3. World Health Organization. The world health report 2002: reducing risks, promoting healthy life. World Health Organization; 2002.
4. Cameron A, Ewen M, Auton M, Abegunde D. The World Medicines Situation 2011. Medicines Prices, Availability and Affordability. World Health Organization; Vol. 3, 2011.
5. Aruru M, Truong H-A, Clark S. Pharmacy Emergency Preparedness and Response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res Social Adm Pharm. 2021;17(1):1967–1977. doi:10.1016/j.sapharm.2020.04.002
6. Goodarzian F, Navaei A, Ehsani B, Ghasemi P, Muñuzuri J. Designing an integrated responsive-green-cold vaccine supply chain network using Internet-of-Things: artificial intelligence-based solutions. Ann Oper Res. 2022;1–45. doi:10.1007/s10479-022-04713-4
7. Goodarzian F, Ghasemi P, Gunasekaren A, Taleizadeh AA, Abraham A. A sustainable-resilience healthcare network for handling COVID-19 pandemic. Ann Oper Res. 2022;312(2):761–825. doi:10.1007/s10479-021-04238-2
8. Bigdeli M, Laing R, Tomson G, Babar Z-U-D. Medicines and universal health coverage: challenges and opportunities. J Pharm Policy Pract. 2015;1–3. doi:10.1186/s40545-014-0024-0
9. Georgiou N, Delfabbro P, Balzan R. COVID-19-related conspiracy beliefs and their relationship with perceived stress and pre-existing conspiracy beliefs. Pers Individ Dif. 2020;166:110201. doi:10.1016/j.paid.2020.110201
10. Edozieuno A. Assessment of anti-malaria logistic management system performance at primary health care level in Oyo state, Nigeria; 2012.
11. Yimenu DK, Demeke CA, Kasahun AE, et al. Impact of COVID-19 on pharmaceutical care services and the role of community pharmacists: a multi-center cross-sectional study in Ethiopia. SAGE Open Nurs. 2021;7:23779608211025804. doi:10.1177/23779608211025804
12. Sheppard J, Thomas CB. Community pharmacists and communication in the time of COVID-19: applying the health belief model. Res Social Adm Pharm. 2021;17(1):1984–1987. doi:10.1016/j.sapharm.2020.03.017
13. Hill A. Ways to safeguard UK drug supplies during COVID-19 and beyond. Pharmaceut J. 2020;304:7936.
14. Hossain MS, Ferdous S, Siddiqee MH. Mass panic during Covid-19 outbreak-A perspective from Bangladesh as a high-risk country. J Biomed Anal. 2020;3(2):1–3. doi:10.30577/jba.v3i2.40
15. Salahuddin M, Manzar D, Unissa A, Pandi-Perumal SR, BaHammam AS. The global shortage of essential drugs during the COVID-19 pandemic: evidence based on aggregated media and social media reports. J Nat Sci Med. 2022;5(1):23.
16. Kebede Y, Birhanu Z, Fufa D, et al. Myths, beliefs, and perceptions about COVID-19 in Ethiopia: a need to address information gaps and enable combating efforts. PLoS One. 2020;15(11):e0243024. doi:10.1371/journal.pone.0243024
17. Kassie BA, Adane A, Tilahun YT, Kassahun EA, Ayele AS, Belew AK. Knowledge and attitude towards COVID-19 and associated factors among health care providers in Northwest Ethiopia. PLoS One. 2020;15(8):e0238415. doi:10.1371/journal.pone.0238415
18. AlRuthia YS, AlKofide H, AlAjmi R, et al. Drug shortages in large hospitals in Riyadh: a cross-sectional study. Ann Saudi Med. 2017;37(5):375–385. doi:10.5144/0256-4947.2017.375
19. Consortium WST. Repurposed antiviral drugs for Covid-19—interim WHO solidarity trial results. N Engl J Med. 2021;384(6):497–511.
20. Kefale AT, Shebo HH. Availability of essential medicines and pharmaceutical inventory management practice at health centers of Adama town, Ethiopia. BMC Health Serv Res. 2019;19(1):1–7. doi:10.1186/s12913-019-4087-0
21. Aronovich DG, Kinzett S. Kenya: Assessment of the Health Commodity Supply Chains and the Role of KEMSA. VA, Arlington: John Snow, Inc; 2001.
22. Fentie M, Fenta A, Moges F, et al. Availability of essential medicines and inventory management practice in primary public health facilities of Gondar town, north West Ethiopia. J PharmaSciTech. 2015;4(2):54–56.
23. Asemahagn MA, Alene GD, Yimer SA. A qualitative insight into barriers to tuberculosis case detection in East Gojjam Zone, Ethiopia. Am J Trop Med Hyg. 2020;103(4):1455. doi:10.4269/ajtmh.20-0050
24. Tumwine Y, Kutyabami P, Odoi RA, Kalyango JN. Availability and expiry of essential medicines and supplies during the ‘pull’and ‘push’drug acquisition systems in a rural Ugandan hospital. Trop J Pharm Res. 2010;9(6):3.
25. Uganda M. Pharmaceutical situation assessment, level II, health facilities survey in Uganda. Ministry of Health; 2008.
26. Ahmed M. Diabetic foot disease and its management. World Fam Med. 2020;18(12):242–247.
27. Zheng S-Q, Yang L, Zhou P-X, Li H-B, Liu F, Zhao R-S. Recommendations and guidance for providing pharmaceutical care services during COVID-19 pandemic: a China perspective. Res Social Adm Pharm. 2021;17(1):1819–1824. doi:10.1016/j.sapharm.2020.03.012
This article has been archived for your research. The original version from Dove Medical Press can be found here.



