Myth and Misinformation on COVID-19 Vaccine | RMHP
Department of Health Informatics, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Mulugeta Hayelom Kalayou, Wollo University, Dessie, Ethiopia, Email [email protected]
Background: To prevent the spread of COVID-19 and carry out a successful vaccination program especially in low-income countries, people must have faith on scientists and health experts. The most significant challenge to vaccination programs’ efficacy is now regarded to be a lack of information and trust in immunization due to myths and misinformation spread in the community. Therefore, this study aimed to identify the myth and misconceptions that are propagated about the COVID-19 vaccine, the refusal rate of the vaccine and determine the factors associated with COVID-19 vaccine refusal.
Methods: A community-based cross-sectional study was conducted from December 7 to January 25, 2022. Face-to-face interviews with a standardized questionnaire were used to collect data on the variables. Data were entered into the statistical tool Epi data version 3.1 and then exported to SPSS version 25 for analysis. Binary logistic regression, both bivariable and multivariable, was conducted. In the multivariable binary logistic regression model, the adjusted odds ratio with 95% confidence interval was used to declare statistically significant factors based on a p value less than 0.05.
Results: Out of the total 574 respondents, 60.3% [95% CI (55.5, 64.2)] of them refused to take COVID-19 vaccine. In this study, respondent’s age [AOR = 2.1 at 95% CI: (1.8, 4.9)], perception on COVID-19 vaccine [AOR = 3.0 at 95 CI: (1.9, 4.6)], eHealth literacy [AOR = 2.7 at 95% CI: (1.7, 4.1)], source of information about the vaccine [AOR = 2.9 at 95% CI: (1.9, 4.4)], computer literacy [AOR = 2.8 at 95 CI: (1.8, 4.2)] and frequency of internet use [AOR = 2.2 at 95 CI: (1.8, 5.3)] were identified as determinant factors for COVID-19 vaccine acceptance.
Conclusion: Factors like eHealth literacy, source of information about the vaccine, frequency of internet use, respondent’s perception about the vaccine and computer literacy were found to be determinant factors for COVID-19 vaccine acceptance.
Introduction
Combating the spread of misinformation, which we define as incorrect or erroneous information conveyed regardless of intent to deceive, is a critical challenge of our day.1–3 The proliferation of disinformation, enabled by many platforms, has the potential to have serious negative repercussions, as individuals become not only uninformed but also less able to believe in scientific truths and trust experts.4–6 Misinformation is connected with moments of political and economic turmoil, and it poses a significant hazard to public health in the COVID-19 pandemic.5–8 Trust in the government, scientists, and health professionals is regarded as critical to avoiding the spread of COVID-19 and executing a successful vaccination campaign.9
Since the first dosage of the COVID-19 vaccine has released to the market, several nations have administered it to the most vulnerable members of society.9–14 The Pfizer COVID-19 vaccine was authorized for use in the United Kingdom on December 2, 2020, with the first dose delivered six days later.15 Initially aimed at adults over the age of 80, those who live or work in nursing homes, and high-risk health-care professionals.9,16 Like other nations of the world, Ethiopia through the Ethiopian Ministry of Health announced the introduction of the COVID-19 vaccine on March 13, 2021, in a high-level national ceremony held at Eka Kotebe COVID-19 Hospital, where frontline health workers were immunized to commemorate the start of the immunization campaign.12 The COVAX initiative, the global community, WHO, and others had provided the vaccines to Ethiopia.12 Since the introduction of the COVID-19 vaccine in Ethiopia around 33.8 million people, only 33% of the total population, were fully vaccinated till July 2022.17
Low vaccination uptake will extend the pandemic’s social and economic effects on families and communities, particularly in low-income nations.18 Like many other regions in low-income countries, the northeast Ethiopia has also paid a lot due to the COVID-19 pandemic.19 Several micro and small business enterprises had left the market due to the inflation occurred by the pandemic. Many elderly and chronic patients had passed away by the pandemic. Many people in developing nations still believe that vaccination is dangerous and unneeded.4 Vaccine hesitancy is one of the top 10 global health issues. According to WHO (2019), the reasons for rejection or unwillingness might be connected to difficulties in obtaining vaccinations, complacency, or a lack of trust, which is a major issue in controlling the virus.20
Even in the United States, during the measles epidemics in California in 2014–2015, around 5–10% of the population held anti-vaccination attitudes.21 Studies conducted in Ethiopia also showed that there is hesitation to receive COVID-19 vaccines.11,13,22–24 The hesitation to receive the COVID-19 vaccine was also found in health care providers that will be a major obstacle for enhancing the vaccination coverage.22,23,25 A survey of Addis Ababa inhabitants found that more over half of those polled had an unfavorable view regarding COVID-19 and its preventative measures. Moreover, one-fifth (19.1%) of individuals were unwilling to be vaccinated when it became accessible.26 Another study conducted among people with chronic illness in Ethiopia showed that around forty percent of the participants were not willing to be vaccinated.27
The biggest threat to the effectiveness of vaccination initiatives is currently thought to be a lack of information and trust in immunization.6 Vaccination reluctance is greatly influenced by many sorts of vaccine information disseminated through the media. Controversies over vaccine safety, which are widely publicized in news headlines, talk programs, and popular publications, also increase vaccine hesitation and anti-vaccination behavior in the community.14,28–32 According to several studies, the heart of anti-vaccine views is a conspiracy notion that vaccinations do not function and/or are actively harmful because they cause many defects to the people who took the vaccine.6,33–35 Some people’s resistance to vaccinations also stems from theological arguments.5,14,34 In the developed world, there are some machine learning and natural language processing algorithm which have been integrated to web extensions for detecting misinformation on COVID-19 vaccines that warns a user of incorrect information when conducting online health searches using a web search engine.36 When it comes to our setting, misinformation in developing countries context is a little bit different from the developed world. Since misinformation is circulated, more in oral based mechanisms than digital platforms.11,25–27
In our setting, even though there are some studies conducted on the willingness to receive COVID-19 vaccine among health workers, there is a limited study on the general population and on the reasons for the refusal of the vaccines. Consequently, the findings from this study will help the stakeholders to act on the identified reasons for vaccination refusals and will help them to tackle the myth and misinformation circulated in the population.
Methods
Study Design and Setting
A community-based cross-sectional study was conducted from December 7 to January 25, 2022. The study was carried out in Dessie, Amhara regional state, Northeast Ethiopia. The city is located in Ethiopia’s Amhara regional state’s South Wollo Zone, 401 kilometers North of Addis Ababa. It is located at 11°8′N 39°38′E and has an elevation of between 2470 and 2550 meters above sea level. The city embraces five sub-cities, which consists 22 Kebeles (the smallest administrative units in Ethiopia). According to Central Statistics Agency (CSA) (2006) projections, Dessie has a total population of 205,000 people, of which 37.8% are children. Dessie is one of the country’s most historic and densely inhabited cities. The city features eight health centers, two government hospitals, three private hospitals, and fifteen clinics, according to the Dessie City administration health office.25
Study Participants
This study’s source population was all people over the age of 18 living in Dessie city, while the study population was people over the age of 18 living in the city’s selected kebeles.
Sampling and Sampling Procedures
The sample size was calculated using a single population proportion formula37 while keeping the following statistical assumptions in mind:
Confidence level (Cl), 95%
Proportion (P) = 50%
Margin of error (W) = 5%, and Z = 1.96, the corresponding Z-score for the 95% CI
Using the single proportion formula below:
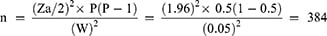
Where n is an initial sample size. The ultimate sample size was 635, based on a 10% non-response rate and a design effect of 1.5. The houses of the participants were visited using the cluster sampling approach. The lottery technique was used to pick eight Kebeles (Kebele 7, Kebele 8, Kebele 9, Kebele 13, Kebele 16, Kebele 17, Kebele 18, Kebele 20) from a total of 22 Kebeles. Then, depending on the number of families, one to two Ketena/s (the lowest administrative cluster) were chosen from each kebele. The chosen Ketena/s were regarded as a cluster, and all homes in the chosen Ketena/s were included. When the parents were not accessible at the time of data collection, either one of the parents or a family member over the age of 18 was questioned in the household.
Operational Definitions
EHealth literacy: the capacity of participants to find and utilize reliable information from the Internet. The participants’ level of eHealth literacy was assessed using a cutoff score of 26, which was used to define their eHealth literacy. Following a study of pertinent literature, we classified eHEALS scores of 26 and below as having low eHealth literacy.38–41
Computer literacy: The degree, to which a person believes he or she can perform a specific task using a computer, was measured using six yes or no questions. Respondents who scored above average were considered as computer literate.22
COVID-19 vaccination acceptance: participants who received vaccine and are willing to take in a future.26
Myth and misinformation on COVID-19 vaccination: Unsubstantiated information circulated in a community, which have a detrimental influence on vaccination uptake in the community.29 The questions were rated using a five-point Likert scale. From strongly disagree to strongly agree.
Data Collection Tools and Procedures
Data were gathered by face-to-face interviews with the use of a standardized questionnaire developed from literature.5,13,14,22,28,40,42,43 The dependent variable was refusal to undergo COVID-19 immunization, while the independent variables were socio-demographic characteristics, technical factors like eHealth literacy, source of COVID-19 information, frequency of internet use and computer literacy.
Data were gathered by BSc Health informatics professionals who were carefully supervised by supervisors who oversaw the whole data collecting procedure. The data collectors and supervisors received a one-day training on the aim of the study, data collecting instruments, collection procedures, and ethical problems during the selection of study participants and data collection. The interviewers manually recorded all replies to closed and open questions. On a daily basis, the supervisors evaluated the consistency and completeness of the data.
Data Management and Analysis
The statistical program Epi data version 3.1 was used for data input, which was subsequently exported to SPSS version 25 for analysis. Descriptive data were provided in the form of narrative and tabulation. Binary logistic regression (bivariable and multivariable) analysis was used to find statistically significant variables associated with vaccination refusal. Variables that in the bivariable analysis had a p-value <0.2 were included in a multivariable model; the adjusted odds ratios (AOR) with 95% confidence interval were reported. The Hosmer and Lemeshow goodness-of-fit test was used and a p-value lower than 0.05 was considered statistically significant.
Ethical Approval
Ethical clearance was obtained from the Institutional Ethical Review Board (IRB) of College of Medicine and Health Sciences of Wollo University (Ref No/CMHS/136/2021) and an official permission letter was gained from the city administrative office. The study was carried out in conformity with the Helsinki Declaration and all subjects gave their informed permission. To ensure anonymity, all identifying concerns were removed. Furthermore, during the data-collecting period, suitable infection prevention procedures and concepts linked to COVID-19 were taken into account. Following the completion of the interview, data collectors offered health education for the family depending on the gaps identified as suitable.
Result
Participants’ Socio-Demographic Characteristics
The current study included 574 study participants, with a response rate of 90.3%. The median age of the study participants was 36 ± 13.24 (SD) years. Three hundred thirty-nine (59.1%) of the research participants were women. Three hundred fifty-eight (59.87%) of the participants in the research were married. In terms of family size, 253 (44.1%) of respondents had more than five family members. Two hundred forty (41.8%) of the study subjects had completed secondary school and above, while 98 (17.1%) had no formal education (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Respondents in Dessie City Administration, Northeast Ethiopia (n=574) |
Myth and Misinformation Circulated in the Community on COVID-19 Vaccine
Among a number of misinformation propagated in the community myths on the efficacy of the drug and the conspiracy notion of the vaccine takes the highest part. Around 147 (25%) of the study participants strongly agreed that COVID-19 pandemic is a conspiracy of pharmaceutical companies to sell products. A total of 226 (39.4%) of the study subjects agreed that the side effects of the COVID-19 vaccines are dangerous. Participants who strongly agreed with a misconception, COVID-19 vaccination being made with or includes questionable chemicals, make up 205 (35.7%) of the entire population. Out of the total participants 378 (65.8%) of them had a misconception on the vaccines effect on women fertility. A total of 274 (47.7%) and 104 (18.1%) of the study subjects Agreed and strongly agreed that the COVID-19 vaccine can affect women’s fertility, respectively. Besides, to the above-mentioned reasons raised by the participants, there is also a theological notion on COVID-19 vaccine. Around half of the participants 242 (42.2%) agreed on the myth about the vaccine, COVID-19 is from God for punishment that could not be prevented by taking vaccines (Table 2).
 |
Table 2 Myth and Misinformation on COVID-19 Vaccines in Northeast Ethiopia (n=574) |
Socio-Demographic Factors Associated with COVID-19 Vaccine Refusal
Participants who were older, greater than the age of 49, had a tendency of accepting the vaccine two times than the respondents whose age were less than thirty [AOR = 2.1 at 95% CI: (1.8, 4.9)]. Respondents with good perception on COVID-19 vaccine were three times more likely to accept the vaccine than their counter parts [AOR = 3.0 at 95 CI: (1.9, 4.6)] (Table 3).
 |
Table 3 Bi-Variable and Multivariable Analysis of Factors Significantly Associated with Acceptance to Be Vaccinated for COVID-19 Vaccine in Northeast Ethiopia, Jan 2022 |
Magnitude of COVID-19 Vaccine Refusal
In this study, the acceptance rate of respondents to the COVID-19 vaccine was 60.3% at 95% CI (55.5, 64.2) (Table 3).
Technological Factors Associated with COVID-19 Vaccine Refusal
In our study, those participants whose eHealth literacy was high were 2.7 times more likely to accept COVID-19 vaccine than those who had a poor eHealth literacy [AOR = 2.7 at 95% CI: (1.7, 4.1)]. Respondents who used information from medical and health institutions accepted COVID-19 vaccine three times than respondents who used non-secular sources [AOR = 2.9 at 95% CI: (1.9, 4.4)]. Respondents who were computer literate were found 2.8 times more likely to accept COVID-19 vaccine than those who were computer illiterate [AOR = 2.8 at 95 CI: (1.8, 4.2)]. Respondents who used internet daily were 2.2 times more likely to accept COVID-19 vaccine than those who used internet one day and less than one day in a week [AOR = 2.2 at 95 CI: (1.8, 5.3)] (Table 3).
Discussion
The purpose of this study was to explore the myth and misinformation of Dessie city administration residents regarding COVID-19 vaccine and their willingness to receive the vaccine. We discovered that participants were exposed to a spread of misinformation, most of which came from social media and non-secular institutions.28,29,31,44 This resulted in confusion, distress, and mistrust in participants’ daily lives about the COVID-19 vaccine. Vaccine refusal could be attributed to three factors: safety concerns, negative stories, and private knowledge, all of which had been exacerbated by recent exposure to misinformation via various platforms. We discovered that the more confused, distressed, and distrustful the participants felt during COVID-19, the more likely they were to be denied the COVID-19 vaccine.
Accordingly, the acceptance of the COVID-19 vaccine for this study was found 60.3% at 95% of CI (55.5, 64.2). The finding was found in agreement with study conducted in Gurage Zone of Ethiopia 62.6%,45 and higher than a studies conducted in Addis Ababa 40%,24 among healthcare providers in Southwestern Ethiopia 48.4%,23 and from the study conducted among the community in Wolaita Sodo of Ethiopia 45.5%.11 The possible reason for having a high acceptance rate of the COVID-19 vaccine compared to the above-mentioned studies could be due to time and enhancement of awareness about the vaccine.
In terms of the factors influencing the outcome variables, socio-demographic variables such as age and perceptions on the COVID-19 vaccine, as well as technical variables such as participants’ information sources for the vaccine, eHealth literacy, frequency of internet use, and computer literacy, had a significant impact on the acceptance of the COVID-19 vaccine. Respondents aged greater than 49 [AOR = 2.1 at 95% CI: (1.8, 4.9)] were accepted COVID-19 vaccine two times than the younger respondents (respondents age less than 30 years). Even though this finding was found aligned with studies conducted in Irish46 and Western India among working-age populations,34 and it is diametrically opposite with the studies conducted in Ethiopia using online survey13 and a cross-sectional study conducted in Pakistan.47 The possible reason for this could be due to young people’s exposure to different COVID-19 related information that makes them uncertain about the vaccine and they tend to think they are invincible.
Concerning the perception of respondents towards the COVID-19 vaccine, respondents with good perception were found three times more likely to accept the vaccine than their counter parts.33,42,48 This might be due to respondents who had poor perception towards the COVID-19 vaccine had a poor perception towards the COVID-19 virus. If participants believed that COVID-19 virus is not a threat for their health and life, their perception to the vaccine would be poor.
Moreover, respondents who had high computer and eHealth literacy were found 2.8 and 2.7 times more likely to accept the COVID-19 vaccine than those who had low computer and eHealth literacy, respectively.7,8,10,49 This might be because computer literacy and eHealth literacy is often used as proxy measure of securing information related to the COVID-19 thereby might have good knowledge and positive attitude towards the vaccine. This finding is indicative for policy makers and intervention strategies to focus on eHealth and computer literacy of community members who have low literacy.
Finally, participants who used internet daily were accepted COVID-19 vaccine two times than those who used internet one day and less than one day in a week. Besides, respondents whose source of information was medical and health information sources were accepted COVID-19 vaccine three times than those who used non-secular sources.5,14,50 The possible reason for this could be that religious beliefs that are preached in the institutions are influencing people’s perception towards the vaccine. Information from non-secular sources like those that vaccines are forbidden by religion (Haram), infidel vaccine or western made vaccine could be their main reason to refuse COVID-19 vaccine.
Conclusion
In our study, around sixty percent of the participants accepted the COVID-19 vaccines. Socio-demographic variables like age and respondent’s perception towards the vaccine were found significant to vaccine acceptance. Technical factors like eHealth literacy, source of information about the vaccine, frequency of internet use and computer literacy were also found determinant factors for COVID-19 vaccine acceptance. We recommended enhancing community’s eHealth and computer literacy and promoting awareness of the reliability of vaccine information sources, as both these actions would help to tackle problems relate to vaccine refusal.
Recommendation for Future Researchers
This study will give a great insight for future researchers to investigate more on myth and misinformation towards vaccine uptake. For the future, we recommend researchers to incorporate qualitative study triangulated with quantitative one.
Limitations of the Study
This study acknowledged some significant potential limitations that should be taken into account when interpreting the findings. First, the study was cross-sectional, which makes establishing cause-effect linkages impossible. Second, there is a chance that social desirability bias will be introduced.
Strength of the Study
Since this survey was conducted using a face-to-face interview and observation with all necessary cautions to prevent contagion the quality of data collected for this study is expected with high quality.
Data Sharing Statement
The corresponding author can provide data to back up the conclusions of this study upon request. Due to privacy and ethical concerns, the data is not publicly available.
Acknowledgment
I would like to thank My Medi/Keyiwa Wef, the study participants, data collectors, supervisors, in addition, the Ethical Review Committee of College of Medicine and Health Sciences of Wollo University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest.
References
1. Farrell J, McConnell K, Brulle R. Evidence-based strategies to combat scientific misinformation. Nat Clim Chang. 2019;9(3):191–195. doi:10.1038/s41558-018-0368-6
2. Koulolias V, Jonathan GM, Fernandez M, Sotirchos D. Combating Misinformation: An Ecosystem in Co-Creation. OECD Publishing; 2018.
3. Safieddine F, Dordevic M, Pourghomi P, editors. Spread of misinformation online: simulation impact of social media newsgroups. 2017 Computing Conference; 2017; IEEE.
4. Dubé E, Laberge C, Guay M, et al. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763–1773. doi:10.4161/hv.24657
5. Perveen S, Akram M, Nasar A, Arshad‐Ayaz A, Naseem A. Vaccination‐hesitancy and vaccination‐inequality as challenges in Pakistan’s COVID‐19 response. J Community Psychol. 2022;50(2):666–683.
6. Ullah I, Khan KS, Tahir MJ, Ahmed A, Harapan H. Myths and conspiracy theories on vaccines and COVID-19: potential effect on global vaccine refusals. Vacunas. 2021;22(2):93–97. doi:10.1016/j.vacun.2021.01.001
7. Nath R, Imtiaz A, Nath SD, Hasan EJV. Role of vaccine hesitancy, ehealth literacy, and vaccine literacy in young adults’ covid-19 vaccine uptake intention in a lower-middle-income country. Vaccines. 2021;9(12):1405. doi:10.3390/vaccines9121405
8. Silva MJ, Santos P, Health P. The impact of health literacy on knowledge and attitudes towards preventive strategies against COVID-19: a cross-sectional study. Int J Environ Res Public Health. 2021;18(10):5421. doi:10.3390/ijerph18105421
9. Trent M, Seale H, Chughtai AA, Salmon D, MacIntyre CR. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: a comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccines. 2021;40:2498–2505.
10. Jarynowski A, Skawina I. Attempt at profiling and regionalisation of COVID-19 vaccine campaigns in Poland–preliminary results. Eur J Transl Clin Med. 2021;4:13–21. doi:10.31373/ejtcm/134674
11. Mesele M, Resistance D. COVID-19 vaccination acceptance and its associated factors in Sodo Town, Wolaita Zone, Southern Ethiopia: cross-sectional study. Infect Drug Resist. 2021;14:2361. doi:10.2147/IDR.S320771
12. World Health Organization. Ethiopia introduces COVID-19 vaccine in a national launching ceremony. World Health Organization; 2021. Available from: https://www.afro.who.int/news/ethiopia-introduces-covid-19-vaccine-national-launching-ceremony. Accessed September 28, 2022.
13. Strupat C, Shigute Z, Bedi AS, Rieger M. Willingness to take COVID-19 vaccination in low-income countries: evidence from Ethiopia. PLoS One. 2022;17(3):e0264633. doi:10.1371/journal.pone.0264633
14. Wirsiy FS, Nkfusai CN, Ako-Arrey DE, et al. Acceptability of COVID-19 vaccine in Africa. Int J Maternal Child Health AIDS. 2021;10(1):134. doi:10.21106/ijma.482
15. Nature. The UK has approved a COVID vaccine — here’s what scientists now want to know; 2020. Available from: https://www.nature.com/articles/d41586-020-03441-8. Accessed September 28, 2022.
16. Chadwick A, Kaiser J, Vaccari C, et al. Online social endorsement and Covid-19 vaccine hesitancy in the United Kingdom. Soc Media+ Society. 2021;7(2):20563051211008817.
17. World Health Organization. Coronavirus disease (COVID-19): vaccines. World Health Organization; 2022. Available from: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-vaccines?gclid=CjwKCAiAprGRBhBgEiwANJEY7Fb52UyP2HX85YgiSUbQNxrYxSnChmKD-IApgQ6N01cCZkEuJFxQYBoCaxkQAvD_BwE&topicsurvey=v8kj13. Accessed September 28, 2022.
18. Kabir R, Mahmud I, Chowdhury MTH, et al. COVID-19 vaccination intent and willingness to pay in Bangladesh: a cross-sectional study. Vaccines. 2021;9(5):416. doi:10.3390/vaccines9050416
19. Goshu D, Ferede T, Diriba G, Ketema M. Economic and welfare effects of COVID-19 and responses in Ethiopia: initial insights; 2020.
20. World Health Organization. Ten threats to global health; 2019. Available from: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. Accessed September 28, 2022.
21. Pananos AD, Bury TM, Wang C, et al. Critical dynamics in population vaccinating behavior. Proc Nat Acad Sci. 2017;114(52):13762–13767. doi:10.1073/pnas.1704093114
22. Ahmed MH, Bogale AD, Tilahun B, et al. Intention to use electronic medical record and its predictors among health care providers at referral hospitals, north-West Ethiopia, 2019: using unified theory of acceptance and use technology 2 (UTAUT2) model. BMC Med Inform Decis Mak. 2020;20(1):1–11. doi:10.1186/s12911-020-01222-x
23. Angelo AT, Alemayehu DS, Dachew AM. Health care workers intention to accept COVID-19 vaccine and associated factors in southwestern Ethiopia, 2021. PLoS One. 2021;16(9):e0257109. doi:10.1371/journal.pone.0257109
24. Sahile AT, Mulugeta B, Hadush S, Fikre EM. COVID-19 vaccine acceptance and its predictors among college students in Addis Ababa, Ethiopia, 2021: a cross-sectional survey. Patient preference and adherence. Pat Preference Adherence. 2022;16:255. doi:10.2147/PPA.S348132
25. Adane M, Ademas A, Kloos H. Knowledge, attitudes, and perceptions of COVID-19 vaccine and refusal to receive COVID-19 vaccine among healthcare workers in northeastern Ethiopia. BMC Public Health. 2022;22(1):1–14. doi:10.1186/s12889-021-12362-8
26. Dereje N, Tesfaye A, Tamene B, et al. COVID-19 vaccine hesitancy in Addis Ababa, Ethiopia: a mixed-methods study. BMJ Yale. 2021;12:e052432.
27. Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting Dessie Comprehensive Specialized Hospital, Northeastern Ethiopia. Patient Prefer Adherence. 2021;15:1795. doi:10.2147/PPA.S324564
28. Donato KM, Singh L, Arab A, Jacobs E, Post D. Misinformation about COVID-19 and Venezuelan migration: trends in Twitter conversation during a pandemic. Harvard Data Sci Rev. 2022. doi:10.1162/99608f92.a4d9a7c7
29. Hayawi K, Shahriar S, Serhani MA, Taleb I, Mathew SS. ANTi-Vax: a novel Twitter dataset for COVID-19 vaccine misinformation detection. Public Health. 2022;203:23–30.
30. Kalayou MH, Tilahun B, Endehabtu BF, Nurhussien F, Melese T, Guadie HA. Information seeking on Covid-19 pandemic: care providers’ experience at the university of Gondar teaching hospital, Northwest of Ethiopia. J Multidiscip Healthc. 2020;13:1957. doi:10.2147/JMDH.S283563
31. O’Neil M, Khan I, Holland K, Cai X. Communication, Society. Mapping the connections of health professionals to COVID-19 myths and facts in the Australian Twittersphere. Info, Commun Society. 2022;1–23. doi:10.1080/1369118X.2022.2032260
32. Yigit M, Ozkaya-Parlakay A, Senel E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. 2021;40(4):e134–e6. doi:10.1097/INF.0000000000003042
33. Sachdeva R. COVID-19 vaccine perceived risks and benefits: scale development and initial tests of the psychometric properties. Am J Health Edu. 2022;53:1–13.
34. Sayed M, Syed H, Guru N, Nazneen S, Sayed S. Hesitancy of COVID-19 vaccine in a working-age population in a town in Central Maharashtra in Western India: a survey based on vaccine characteristics. Int J Infect Dis. 2022;116:S62. doi:10.1016/j.ijid.2021.12.146
35. Medicine JH. COVID-19 vaccines: myth versus fact; 2022. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/covid-19-vaccines-myth-versus-fact. Accessed September 28, 2022.
36. Shams AB, Hoque Apu E, Rahman A, et al. Web search engine misinformation notifier extension (SEMiNExt): a machine learning based approach during COVID-19 Pandemic. Healthcare. 2021;9:156.
37. Lwanga SK, Lemeshow S. Sample Size Determination in Health Studies: A Practical Manual. World Health Organization; 1991.
38. Milne RA, Puts MT, Papadakos J, et al. Predictors of high eHealth literacy in primary lung cancer survivors. J Cancer Edu. 2015;30(4):685–692. doi:10.1007/s13187-014-0744-5
39. Mitsutake S, Shibata A, Ishii K, Okazaki K, Oka K. Developing Japanese version of the eHealth literacy scale (eHEALS). Jpn J Public Health. 2011;58(5):361–371.
40. Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. 2006;8(4):e507. doi:10.2196/jmir.8.4.e27
41. Van der Vaart R, Van Deursen AJ, Drossaert CH, Taal E, van Dijk JA, van de Laar MA. Does the eHealth Literacy Scale (eHEALS) measure what it intends to measure? Validation of a Dutch version of the eHEALS in two adult populations. J Med Internet Res. 2011;13(4):e1840.
42. Marzo RR, Ahmad A, Islam MS, et al. Perceived COVID-19 vaccine effectiveness, acceptance, and drivers of vaccination decision-making among the general adult population: a global survey of 20 countries. PLoS Negl Trop Dis. 2022;16(1):e0010103. doi:10.1371/journal.pntd.0010103
43. Tao L, Wang R, Han N, et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi-center cross-sectional study based on health belief model. Hum Vaccin Immunother. 2021;17(8):2378–2388. doi:10.1080/21645515.2021.1892432
44. Challenger A, Sumner P, Bott L. COVID-19 myth-busting: an experimental study. BMC Public Health. 2022;22(1):1–13. doi:10.1186/s12889-021-12464-3
45. Abebe H, Shitu S, Mose AJI. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. Infect Drug Resist. 2021;14:2015. doi:10.2147/IDR.S312116
46. Association TIPH. About 9% of younger people refusing Covid-19 vaccine, survey finds: the Irish Times; 2022. Available from: https://www.irishtimes.com/news/health/about-9-of-younger-people-refusing-covid-19-vaccine-survey-finds-1.4709622. Accessed September 28, 2022.
47. Samo AA, Sayed RB, Valecha J, Baig NM, Laghari ZA. Immunotherapeutics. Demographic factors associated with acceptance, hesitancy, and refusal of COVID-19 vaccine among residents of Sukkur during lockdown: a cross sectional study from Pakistan. Hum Vaccin Immunother. 2022;18:1–5.
48. Coe AB, Elliott MH, Gatewood SB, Goode J-VR, Moczygemba LR, Pharmacy A. Perceptions and predictors of intention to receive the COVID-19 vaccine. Res Soc Administrat Pharm. 2022;18(4):2593–2599. doi:10.1016/j.sapharm.2021.04.023
49. Basch CH, Meleo-Erwin Z, Fera J, Jaime C, Basch CE. Immunotherapeutics. A global pandemic in the time of viral memes: COVID-19 vaccine misinformation and disinformation on TikTok. Hum Vaccin Immunother. 2021;17(8):2373–2377. doi:10.1080/21645515.2021.1894896
50. Dhama K, Sharun K, Tiwari R, et al. COVID-19 vaccine hesitancy–reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Hum Vaccin Immunother. 2021;17(10):3495–3499. doi:10.1080/21645515.2021.1926183