Post Omits Paxlovid’s Ability to Protect Against Severe COVID-19, Death
SciCheck Digest
Paxlovid, Pfizer’s COVID-19 antiviral pill, has been shown to prevent severe COVID-19 and death. An online post alleging the drug is a “fraud” and “should be taken off the market” neglects to mention this important information, and falsely says ivermectin is superior.

Full Story
A randomized controlled trial and real-world studies have found that for certain patients, Paxlovid, Pfizer’s COVID-19 antiviral pill, reduces the risk of COVID-19 and death.
The Food and Drug Administration authorized the drug for outpatients “at high risk for progression to severe COVID-19” last December, based on a randomized controlled trial that found the medication to be about 88% effective in preventing hospitalization and death in unvaccinated, high-risk adults with COVID-19.
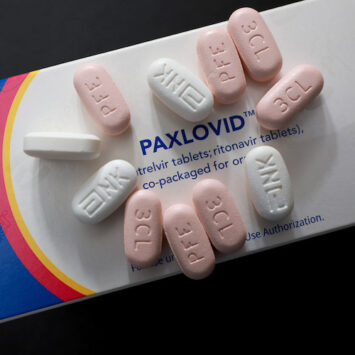
High-risk people with mild to moderate COVID-19 are eligible to take a five-day course of Paxlovid, as long as they start the pills within five days of symptom onset. Paxlovid consists of two sets of tablets that are taken together: nirmatrelvir, a new protease inhibitor that prevents replication of the coronavirus, and ritonavir, an existing drug that boosts levels of nirmatrelvir in the blood.
Several observational studies have subsequently found that Paxlovid is effective in the real world, particularly for older, high-risk people and those who are unvaccinated, but also for some vaccinated people.

An online post being shared on social media, however, claims that the drug is a “fraud” and “should be taken off the market.” After highlighting high-profile cases of COVID-19 rebound after taking Paxlovid, among other issues, the post directs people to use unsupported treatments for COVID-19, including ivermectin, which it falsely says is “very effective” and better than Paxlovid.
“Remember, when it comes to COVID-19, early treatment is crucial, and effective protocols are readily available — just not from the FDA, CDC or even most hospitals,” the post reads.
This is dangerously wrong advice. While there are legitimate concerns about rebound — a situation in which patients recover but then test positive or have symptoms again — and questions about how widely Paxlovid should be described, the drug is a preferred therapy for COVID-19 that has been shown to save lives. Ivermectin, by contrast, has repeatedly failed in trials to benefit COVID-19 patients.
The post is authored by Dr. Joseph Mercola, an osteopathic physician and natural health proponent, and appears on the website for Children’s Health Defense, Robert F. Kennedy’s anti-vaccine group. Both are frequent sources of misinformation about COVID-19 and other health topics.
The FDA has issued warning letters to Mercola, who sells dietary supplements on his website, for misleadingly representing certain products as safe and/or effective in treating or preventing diseases, including COVID-19.
Misleading Description of Paxlovid
Mercola’s article argues that because Paxlovid “is widely associated with rebound infection, and people who take the treatment can still transmit COVID-19 to others,” it should be pulled from the market.
But drugs do not need to prevent viral transmission to be considered a success — and that’s not why Paxlovid was authorized for COVID-19. It was authorized because a randomized controlled trial found that unvaccinated, high-risk people who had not been previously infected were much less likely to be hospitalized for COVID-19 or die when taking the pills, compared with those who didn’t. The final trial result found that the risk of hospitalization or death was 86% lower when taking Paxlovid.
Subsequent observational studies in the real world have borne out those basic findings. One study, published in October in the Lancet, found that when a BA.2 omicron subvariant was dominant in Hong Kong, Paxlovid was associated with a 66% lower risk of death and 24% lower risk of hospitalization among a mostly older (60 years and above) or unvaccinated population, compared with those given no antiviral treatment.
An unpublished study of patients 50 years and older in Massachusetts and New Hampshire similarly found the risk of hospitalization after a COVID-19 diagnosis during an omicron wave was 45% lower among those prescribed Paxlovid, with greater reductions among those who were unvaccinated or obese.
An Israeli study published in June identified a 46% lower risk of severe COVID-19 or death among high-risk adults taking Paxlovid, regardless of vaccination status. The analysis further suggested that the drug was more effective in people 60 years and older, those with cardiovascular and neurological diseases, and immunosuppressed people.
Another Israeli study, published in August in the New England Journal of Medicine, found that for people 65 years and older, the risk of COVID-19 hospitalization and death was significantly lower among those who received Paxlovid, although there was no such benefit in younger people ages 40 to 64.
None of this is mentioned in Mercola’s article. (Another study, published after Mercola’s article was posted, also found Paxlovid was associated with a 51% lower rate of COVID-19 hospitalization among American adults, including vaccinated and previously infected adults.) Nor does the post explain that according to the National Institutes of Health COVID-19 treatment guidelines, Paxlovid is the preferred treatment for patients who aren’t hospitalized.
Monoclonal antibodies, which once worked quite well, do not appear effective against the latest omicron subvariants, and Paxlovid has consistently outperformed the other oral antiviral, molnupiravir.
“Paxlovid is kind of the primary thing,” Dr. David Boulware, an infectious disease physician-scientist at the University of Minnesota who has studied COVID-19 treatments, told us in a phone interview. “It’s an important therapy. For people who are immunocompromised, people at high risk of serious complications, it’s going to be the preferred drug.”
Paxlovid, of course, is not perfect. Some patients with liver or kidney disease or those already taking certain medications should not take it, although many of the dangerous drug interactions can be avoided if people temporarily stop taking the problematic medications.
And other than the original population studied in the randomized clinical trial, it’s still not clear exactly who benefits from taking Paxlovid. As we’ve written, there is a debate about how widely Paxlovid should be prescribed, particularly for younger or lower-risk individuals and people who have been vaccinated or previously infected with the coronavirus, as the benefits are either less clear or less substantial.
Pfizer’s clinical trial testing Paxlovid among “standard risk” people, which initially included vaccinated higher-risk adults with at least one risk factor for severe disease as well as unvaccinated people at low risk, did not meet its primary endpoint of sustained alleviation of all symptoms for four consecutive days.
Among vaccinated higher risk people in the trial, there was a 57% reduction in COVID-19 hospitalization or death, but this result was not statistically significant because there were very few hospitalizations or deaths in either the placebo or Paxlovid groups. Another subanalysis suggested that the drug may have reduced the number of daily medical visits of all types, including telehealth appointments — a result that’s unlikely to be compelling to most people.
“There is some truth to the fact that it’s probably overprescribed,” Boulware said, of Paxlovid being given to people who might formally fit the definition the CDC uses for high risk, but are actually still at low risk, such as a 25-year-old with asthma.
Boulware said he thought there was only a small benefit of Paxlovid even in vaccinated older people, in part because the vaccines work so well.
“But it certainly does have a benefit in people who are elderly, who are immunocompromised, who are not vaccinated, who have not had prior infection,” he added.
As for the claim about not stopping viral transmission, Boulware said that in theory, because the drug reduces the viral load in people, Paxlovid would be expected to reduce — but not eliminate — transmission, although there isn’t data on that yet.
COVID-19 Rebound
Much of Mercola’s post is focused on COVID-19 rebound, or a resurgence in a person’s viral load, which can cause someone to test positive after testing negative, sometimes accompanied by a recurrence of symptoms. The article details several examples of public figures, including President Joe Biden, Dr. Anthony Fauci and CDC Director Dr. Rochelle Walensky, who experienced rebound after taking Paxlovid.
As we’ve written, many experts believe the rebound phenomenon is more likely after taking Paxlovid, but it’s still unknown how frequent it is — and rebound does happen in the absence of uPaxlovid.
Pfizer told us in a statement that the company believes rebound “is uncommon and not uniquely associated with any specific treatment.”
The company reported in an unpublished study in June that in its main trial, the viral loads of COVID-19 patients rebounded after treatment in 7.0% of Paxlovid recipients and 4.1% of placebo recipients. Both arms of the trial included nearly 1,000 people.
A preliminary, unpublished study released this month suggests the rebound rates could be higher, with or without Paxlovid. The study prospectively followed 170 people who tested positive for COVID-19 and were eligible to take Paxlovid. It found that 14.2% of people who chose to receive Paxlovid and 9.3% of people who opted not to take the drug tested positive again on an antigen test, with 18.9% of people taking Paxlovid and 7.0% of those who didn’t experiencing a recurrence of symptoms. While the results point toward rebound being more common after taking the drug, the study was too small and not statistically powered to identify differences between the groups.
As evidence of rebound being a problem, the post cites a CDC advisory from May that describes COVID-19 rebound after Paxlovid treatment. But Mercola neglects to mention that the agency explicitly states in boldface that the drug “continues to be recommended.”
For people who are not truly high risk — and are unlikely to benefit much from Paxlovid — Boulware said the heightened risk of rebound is a valid reason not to take the drug. But it should not dissuade those for whom the medication is most likely to help.
COVID-19 rebound could be annoying and prolong how long someone needs to isolate, but does not appear to lead to severe illness.
“We advise patients of the possibility of rebound with nirmatrelvir-ritonavir, but for patients at risk for progression to severe disease (such as those with advanced age or multiple comorbidities), the potential benefits of treatment greatly outweigh any potential inconvenience from rebound,” the authors of an UpToDate review on the topic wrote. “By contrast, we do not use nirmatrelvir-ritonavir simply to shorten the duration of viral shedding in people who are not at high risk for progression, as the possibility of rebound negates this effect.”
As for the many high-profile rebound cases, Mercola’s examples are factual, but the anecdotes are probably not representative. Boulware suspects that one issue at play is the timing of Paxlovid treatment. If the medication is given very early after diagnosis, as it often is for high-profile politicians and physicians, he said, rebound might be more likely.
“I think [for] the average person, where it takes them a couple days to get a diagnosis, talk to a doctor, call in a prescription and go to the pharmacy, rebound is less common,” he said.
False Claims About Remdesivir and Ivermectin
While misleadingly calling Paxlovid a “fraud,” Mercola also makes false claims about other drugs.
He incorrectly says that remdesivir, an intravenous antiviral approved for COVID-19, “routinely causes severe organ damage and, often, death,” and asserts that ivermectin, an antiparasitic medication, “has been very effective against COVID-19 and shown to outperform at least 10 other drugs, including Paxlovid.”
Boulware said both claims were false. As we’ve written, clinical trials have not found remdesivir is hazardous to COVID-19 patients. Patients receiving remdesivir need to be monitored, and the drug should not be used in some patients with kidney disease, for example. But that does not mean the drug cannot be safely used.
The study Mercola cites for the claim, a small randomized controlled trial conducted in China in early 2020 and published in the Lancet, concluded that remdesivir was “adequately tolerated.” While more patients in the remdesivir than the placebo group discontinued the drug due to adverse events, a similar percentage of patients in both groups experienced adverse events or died. “All deaths during the observation period were judged by the site investigators to be unrelated to the intervention,” the paper reads.
Boulware said remdesivir is not being used much for outpatient therapy anyway, since it must be administered intravenously.
The notion that ivermectin is highly effective against COVID-19 and is better than Paxlovid is also incorrect. Large, placebo-blinded randomized controlled trials have repeatedly failed to identify meaningful clinical benefits of ivermectin against COVID-19, as we’ve written.
Mercola misleadingly cites a computational study for his claim about ivermectin’s superiority. Using computer modeling to estimate the ability of 10 “promising” drugs to bind to a critical coronavirus protein, the authors found that ivermectin “showed the highest binding affinity,” which they say suggests ivermectin could be the “most effective drug candidate.” But the authors also say that “further research is crucial to authenticate these statements.”
Indeed, a computer-based protein binding study does not trump the numerous clinical studies that tell us how the two drugs perform in people, which clearly show Paxlovid as the superior therapy.
Editor’s note: SciCheck’s COVID-19/Vaccination Project is made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation. The goal of the project is to increase exposure to accurate information about COVID-19 and vaccines, while decreasing the impact of misinformation.
Sources
“Coronavirus (COVID-19) Update: FDA Authorizes First Oral Antiviral for Treatment of COVID-19.” Press release. FDA. 22 Dec 2021.
“Ritonavir-Boosted Nirmatrelvir (Paxlovid).” COVID-19 Real Time Learning Network. Infectious Diseases Society of America. Accessed 23 Nov 2022.
Hammond, Jennifer et al. “Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19.” NEJM. 16 Feb 2022.
McDonald, Jessica. “Q&A On Paxlovid, Pfizer’s COVID-19 Oral Antiviral.” FactCheck.org. Updated 27 May 2022.
“COVID-19 Treatment Guidelines.” National Institutes of Health. Accessed 23 Nov 2022.
Archived FDA Warning Letter to Joseph Mercola. 16 Feb 2005.
Archived FDA Warning Letter to Joseph Mercola. 21 Sep 2006.
FDA Warning Letter to Mercola.com, LLC. FDA. 18 Feb 2021. Accessed 23 Nov 2022.
“Pfizer Announces Submission of New Drug Application to the U.S. FDA for PAXLOVID.” Press release. Pfizer. 30 Jun 2022.
“Information Sheet – Paxlovid Eligibility and Effectiveness.” Administration for Strategic Preparedness & Response. HHS. August 2022.
Wong, Carlos K. H. et al. “Real-world effectiveness of molnupiravir and nirmatrelvir plus ritonavir against mortality, hospitalisation, and in-hospital outcomes among community-dwelling, ambulatory patients with confirmed SARS-CoV-2 infection during the omicron wave in Hong Kong: an observational study.” Lancet. 8 Oct 2022.
Dryden-Peterson, Scott et al. “Nirmatrelvir plus ritonavir for early COVID-19 and hospitalization in a large US health system.” medRxiv. 17 Jun 2022.
Najjar-Debbiny, Ronza. “Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients.” Clinical Infectious Diseases. 2 Jun 2022.
Arbel, Ronen et al. “Nirmatrelvir Use and Severe Covid-19 Outcomes during the Omicron Surge.” NEJM. 24 Aug 2022.
Shah, Melisa M. et al. “Paxlovid Associated with Decreased Hospitalization Rate Among Adults with COVID-19 — United States, April–September 2022.” MMWR. 22 Nov 2022.
NIH COVID-19 Treatment Guidelines. “The COVID-19 Treatment Guidelines Panel’s Statement on Omicron Subvariants, Pre-Exposure Prophylaxis, and Therapeutic Management of Nonhospitalized Patients With COVID-19.” 10 Nov 2022.
Boulware, David. Professor of Medicine, Division of Infectious Diseases and International Medicine at the University of Minnesota. Phone interview with FactCheck.org. 15 Nov 2022.
“Merck and Ridgeback Biotherapeutics Provide Update on New Clinical and Non-Clinical Studies of LAGEVRIO™ (molnupiravir).” Press release. Merck. 6 Oct 2022.
“Side-by-Side Overview of Therapeutics Authorized or Approved for the Prevention of COVID-19 Infection or Treatment of Mild to Moderate COVID-19.” HHS Theraputics Team. Oct 2022.
“Pfizer Reports Additional Data on PAXLOVID™ Supporting Upcoming New Drug Application Submission to U.S. FDA.” Press release. Pfizer. 14 Jun 2022.
Rubin, Rita. “From Positive to Negative to Positive Again—The Mystery of Why COVID-19 Rebounds in Some Patients Who Take Paxlovid.” JAMA. 8 Jun 2022.
Pfizer. Statement emailed to FactCheck.org. 17 Nov 2022.
Soares, Holly et al. “Viral Load Rebound in Placebo and Nirmatrelvir-Ritonavir Treated COVID-19 Patients is not Associated with Recurrence of Severe Disease or Mutations.” Research Square preprint. 21 Jun 2022.
Pandit, Jay A. et al. “The Paxlovid Rebound Study: A Prospective Cohort Study to Evaluate Viral and Symptom Rebound Differences Between Paxlovid and Untreated COVID-19 Participants.” medRxiv. 15 Nov 2022.
“COVID-19 Rebound After Paxlovid Treatment.” Health Alert Network. CDC. 24 May 2022.
Smith, Davey M. et al. “Recurrence of Symptoms Following a 2-Day Symptom Free Period in Patients With COVID-19.” JAMA Network Open. 27 Oct 2022.
Cohen, Pieter and Kelly Gebo. “COVID-19: Management of adults with acute illness in the outpatient setting.” UpToDate. Accessed 23 Nov 2022.
Hale Spencer, Saranac. “Clinical Trials Find No Increase in Mortality Among COVID-19 Patients Treated with Remdesivir, Contrary to Viral Claim.” FactCheck.org. 6 Apr 2022.
“Remdesivir.” NIH COVID-19 Treatment Guidelines. Accessed 23 Nov 2022.
Wang, Yeming et al. “Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial.” The Lancet. 16 May 2020.
Parvez, Md Sorwer Alam et al. “Insights from a computational analysis of the SARS-CoV-2 Omicron variant: Host–pathogen interaction, pathogenicity, and possible drug therapeutics.” Immunity, Inflammation and Disease. 21 Jun 2022.

