New Disease VEXAS Syndrome Manifests After COVID and Vaccination
Symptoms of VEXAS syndrome, first discovered in 2020, are highly variable and nonspecific.
Some vaccinated and COVID-infected people are reportedly being diagnosed with a new type of disease called VEXAS syndrome—an autoinflammatory disease discovered in 2020.
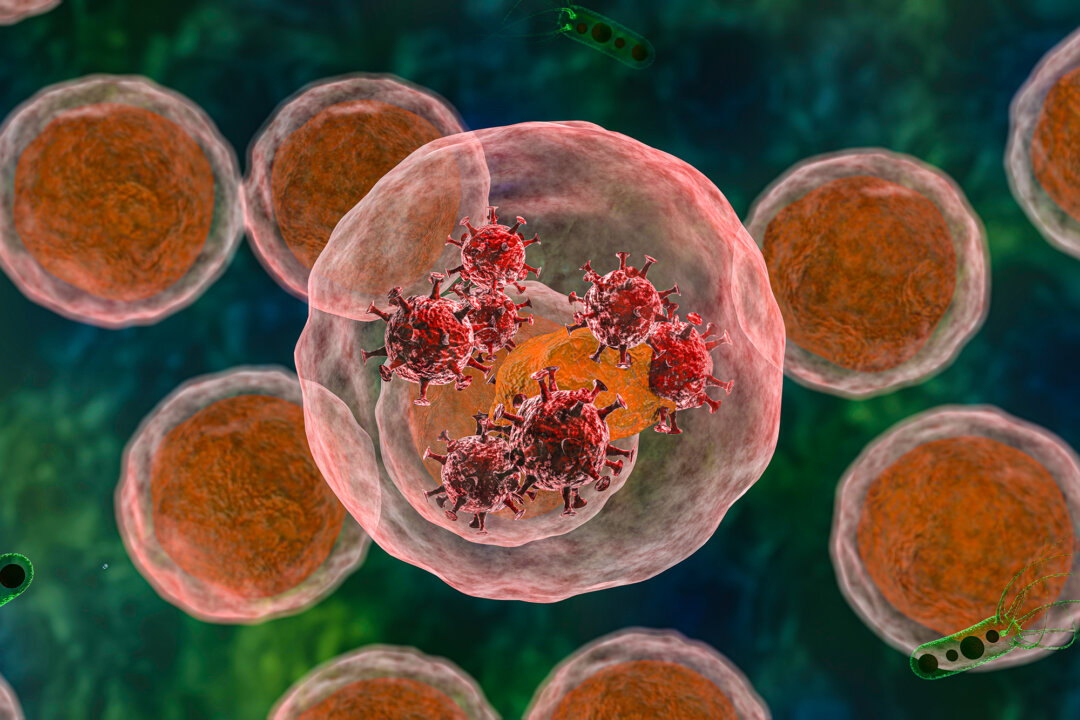
Many people are familiar with autoimmune diseases, often caused by dysfunction among the adaptive immune cells, while problems within the innate immune system often cause autoinflammatory diseases.
VEXAS syndrome—short for vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic syndrome—is caused by mutations in the innate immune cells, a somatic mutation in the UBA1 gene found on the X chromosome.
Somatic mutations cannot be inherited, meaning individuals acquire this mutation later in life.
The mutation affects the stem cells in the bone marrow. The cells mature into specialized immune cells that circulate within the bloodstream.
Immune cells carrying the UBA1 mutation are highly inflammatory, and once enough of them accumulate, patients start developing symptoms.
Three days after receiving the Pfizer COVID vaccine, the man developed tender bumps under the skin, rashes, and purple spots on his limbs. Skin problems are commonly reported in VEXAS patients. He was later determined to have the UBA1 mutation.
“The rare incidence of VEXAS syndrome and the short delay of 3 days between vaccination and onset of symptoms were very suggestive of the vaccine role as a trigger,” authors from Drôme Nord Hospitals wrote.
For months, clinicians misdiagnosed him as having long COVID. However, the patient was diagnosed with VEXAS syndrome upon detecting the UBA1 mutation.
Some doctors say there may be a link but an indirect one.
“In my experience, it is unlikely that VEXAS syndrome could have been triggered by an infection or COVID-19 vaccination,” Dr. Sinisa Savic, immunologist and associate clinical professor at the University of Leeds, told The Epoch Times.
“We know that as people age, they develop all sorts of mutations in the bone marrow … That is why VEXAS is largely found in the elderly population,” he added.
VEXAS syndrome tends to manifest in older men over 50.
However, infections and vaccinations can trigger or worsen symptoms in people already on track to develop VEXAS syndrome, Dr. Savic said.
“Anything that triggers an immune response can cause temporary worsening symptoms; I don’t think there’s any particular argument about that.”
Immune Reactions Worsen Autoinflammatory Diseases
Among the specialized immune cells, only the innate immune cells have been found to carry the mutation. The adaptive immune cells, forming what is known as the “third” or last line of defense, have not been found to carry this mutation.
Dr. Savic said it is possible that adaptive immune cells—T and B cells—would be unable to survive long enough to become specialized if they carry the UBA1 mutation, while specialization of innate immune cells appears to be less affected by the UBA1 mutation.
All infections and vaccinations trigger immune responses necessary for the immune system to react and form immune memory to the pathogen.
However, for patients suffering from autoinflammatory diseases, any immune reaction can cause an imbalance in an already precarious system, potentially worsening the patient’s conditions, according to Dr. Savic.
“This is the case with any autoimmune or inflammatory condition because the immune system tries to control itself, but if you’re then challenged by something else, then that level of control may be reduced,” he said.
During an immune response, the body produces more immune cells; in patients with VEXAS syndrome, this could mean more mutated innate cells.
Innate immune cells are also the first line of defense; they are the first immune cells to activate.
Symptoms Highly Variable, Could Potentially ‘Cause Damage to Everything’
VEXAS syndrome was first detected in 2020. Researchers from the National Institutes of Health (NIH) recruited over 2,500 patients suffering from various inflammatory diseases and studied their genes for shared mutation.
Three patients were found to have UBA1 mutation, which the authors linked to their inflammatory manifestation. Since then, hundreds of people with VEXAS syndrome have been identified by the NIH and around the world.
Symptoms of VEXAS syndrome are highly variable and nonspecific, Dr. Savic said.
Patients may develop weight loss, fever, malaise, skin rashes, and joint and tissue inflammation. Since the disease affects immune cells in the blood, many people may have anemia and insufficient immune cells in circulation.
In the bone marrow, mutated stem cells produce specialized yet mutated immune cells with vacuoles that look “completely disorganized” under the microscope. They also “produce quite significant amounts of inflammatory chemicals,” Dr. Savic said.
These specialized immune cells then enter into the circulation, inducing inflammation in the body.
As the disease progresses, different organs become inflamed and impaired and may start to fail, causing death.
It has not been proven without a doubt, Dr. Savic said, but “there is certainly an agreement in opinion that most of the organ inflammation is caused by these mutated cells infiltrating the organ and causing damage to everything.”
Many patients also develop progressive bone marrow failure, which can also lead to death if untreated.
However, the prognosis of patients varies; some decline rapidly, while others with similar biometrics may survive for many years.
Limited Treatment for VEXAS Syndrome
Since the disease was only recently discovered, researchers have not found many viable long-term treatments.
Patients usually respond well to anti-inflammatory steroids, but steroids are harmful if used for prolonged periods.
Patients at risk of bone marrow failure may be considered for allogeneic stem cell transplant. In this procedure, the body’s stem cells are destroyed using chemo and radiation therapy and replaced with another person’s stem cells.
Autologous transplants, meaning transplantation of the person’s own healthy stem cells, are often not considered out of concern that mutated cells may be transplanted.
However, Dr. Savic said that there have been cases of successful autologous transplants where the patient with VEXAS syndrome was cured. These transplantations, however, took place before the patient was diagnosed with VEXAS syndrome.
While clinicians have not found better treatments for their patients, they at least have a clearer idea of what not to give them.
“In the past, many of these patients would have been on treatments that are so-called traditional DMARDs (disease-modifying antirheumatic drugs), which are to a degree bone marrow toxic, and in these circumstances certainly wouldn’t be the conditions you would want to use,” Dr. Savic explained.
Many patients found not to have the UBA1 mutation still have symptoms that look very similar to those of VEXAS syndrome.
This article has been archived for your research. The original version from Epoch Times can be found here.