4 Experts Discuss Medical Mistrust in Clinical Trials: Honoring the Past, Embracing the Future
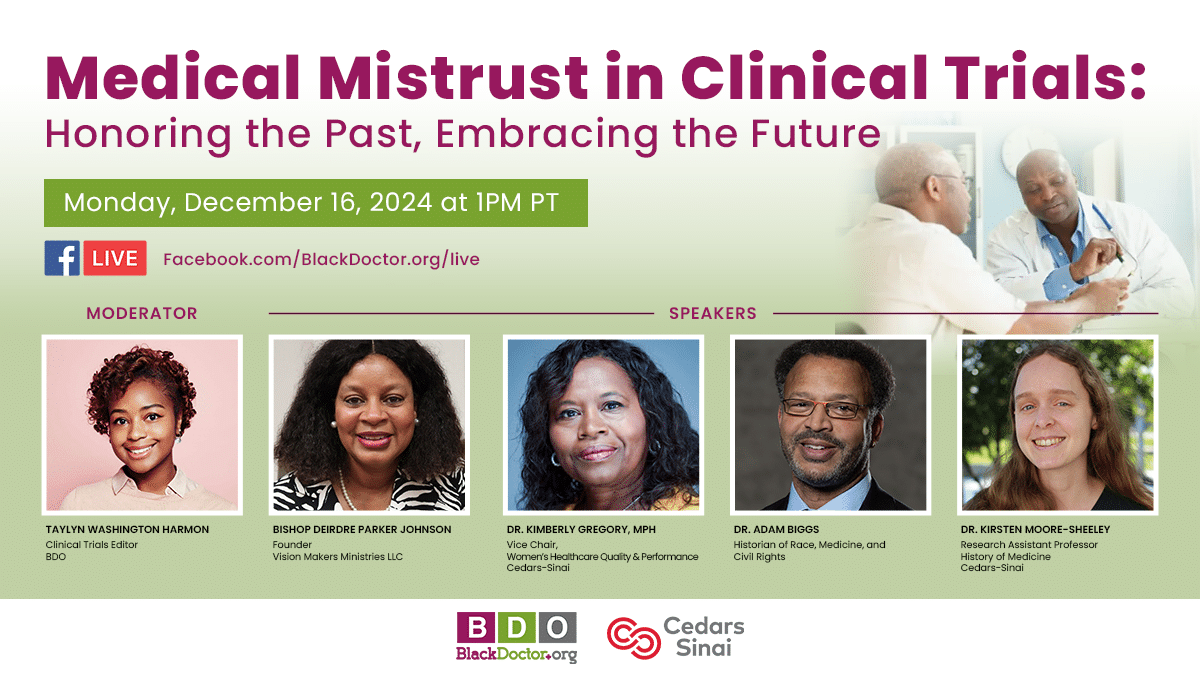
A panel of medical and historical experts recently gathered to discuss the complex issue of medical mistrust in clinical trials among Black Americans, exploring the historical roots of this mistrust and ways to rebuild trust and encourage participation going forward.
The panel, hosted by BlackDoctor.org, included Dr. Bishop Deirdre Parker Jackson, whose grandfathers were victims of the infamous Tuskegee syphilis study; Dr. Kimberly Gregory, vice chair of Women’s Healthcare Quality and Performance Improvement in the Department of Obstetrics and Gynecology at Cedars-Sinai; Dr. Adam Biggs, a historian of race and medicine at Rensselaer Polytechnic Institute; and Dr. Kirsten Moore-Sheeley, a research professor in the history of medicine at Cedars-Sinai.
The Historical Context of Medical Mistrust
The panelists emphasized the importance of understanding the historical context behind medical mistrust. Dr. Parker Jackson explained how the unethical Tuskegee study, conducted from 1932-1972, continues to impact trust today:
“For over 52 years, a signal has been placed on the city of Tuskegee and Tuskegee University because of the unethical study that took place for 30 years from 1932 to 1972,” she said. “Whenever someone says something about the study of syphilis, they say Tuskegee.”
Dr. Biggs added that medical exploitation of Black Americans was more widespread than just the Tuskegee study, noting it was “much more normative in the profession than we’d often like to acknowledge.”
Rebuilding Trust and Encouraging Participation
The experts discussed ways to rebuild trust and encourage participation in clinical trials today. Dr. Gregory emphasized the importance of building relationships:
“If you’re gonna ask somebody to be in your study, they should be paid to be in your study,” she said. “There are a lot of things that are forced into our system because that’s what the medical system wants. That isn’t conducive to the participant. And the more we engage them and include them in the planning, the more likely we’ll be able to solve some of those barriers.”
Dr. Moore-Sheeley stressed the need for ongoing community engagement: “Continuing to maintain relationships and engagement after clinical trials are over, I think, is also very important. So you don’t perpetuate this idea that, oh, well, we had this time-limited kind of access to healthcare through this trial, and now the investigators have forgotten about me, have forgotten about us.”
Transparency and Accountability
The panelists also discussed the importance of medical institutions’ transparency. Dr. Biggs argued that universities and research institutions need to acknowledge past wrongdoings: “We have to be authentic. We have to be forthright. We have to, I mean, essentially, be repentant about our complicity in these things if we want people to actually trust us or have a reason to trust us,” he said.
Dr. Parker Jackson emphasized that everyone has a role to play in rebuilding trust and encouraging participation in clinical trials: “All of us are responsible whether we are in the medical industry or not, but definitely the medical industry,” she said. “We are responsible for conducting research. We are responsible for making sure that we don’t put out false information.”
The Importance of Questioning and Safeguards
The experts agreed that asking questions and maintaining healthy skepticism is crucial. Dr. Biggs encouraged “rigorous critical self-reflection” when considering participation in clinical trials.
Dr. Gregory reminded viewers that there are ethical safeguards in place for modern clinical trials: “There is what, an institutional review board, an IRB, where all clinical trials have to, you know, meet a minimum standard of, an audience of not only subject matter experts, but most IRBs actually also have community members who are representative of the lay public.”
In closing, the panelists emphasized the ongoing importance of medical research while acknowledging the need to address broader healthcare inequities. As Dr. Moore-Sheeley noted:
“Some of the issues of mistrust and distrust in clinical trials is very much connected to issues with the larger healthcare system in terms of access, you know, not only to doctors, but then to therapies after… And so I think it might behoove us to think about this issue, not just in isolation in terms of medical research, but how can we address this issue in conjunction with some of these larger issues, with inequities in the healthcare system more broadly.”
