I study diet and chronic illness. Here’s the uncomfortable truth about seed oils
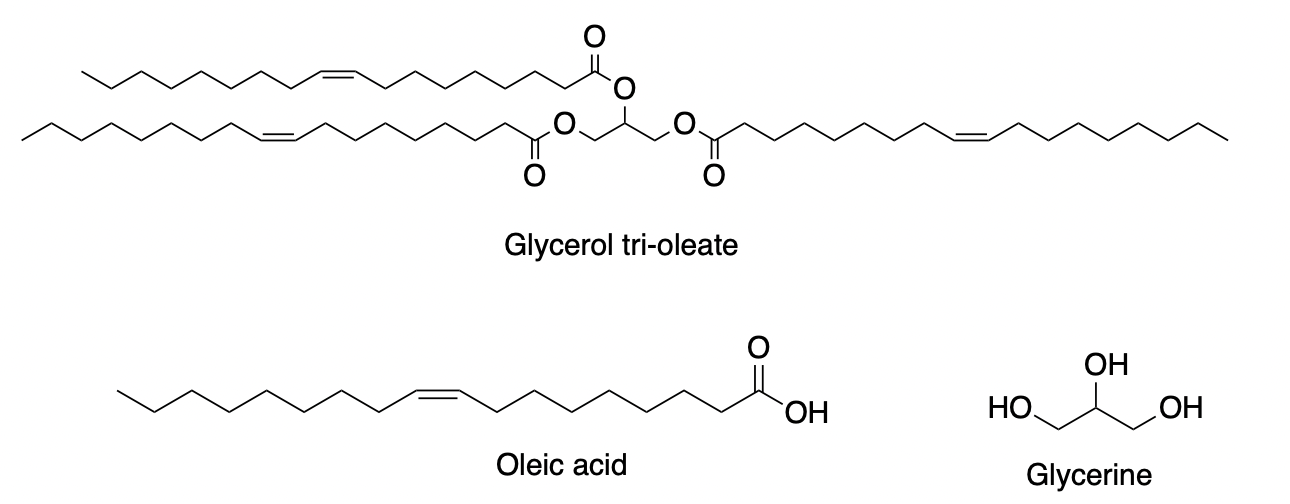
For decades, mainstream nutrition guidelines have recommended that Americans replace animal fats like butter or lard with polyunsaturated fats, especially seed oils such as soybean, corn, and sunflower oils. These oils are rich in omega-6 fatty acids and now make up a significant portion of the fat consumed in the standard American diet.
But recently, the conversation has shifted. Some high-profile figures, including Health and Human Services Secretary Robert F. Kennedy Jr., have claimed that seed oils are harmful and promote inflammation and chronic disease. Critics of seed oils are often accused of spreading fear or misinformation — and sometimes those concerns are justified. But here’s the uncomfortable truth: The scientific community has not definitively determined the health effects of high seed oil consumption. And the current evidence is not as conclusive or unidirectional as many assume.
I say this as a researcher who has been studying diet, genetics, and chronic disease for more than 10 years. When I first entered this field, I assumed the science around dietary fats was largely settled. So I was surprised to see how much disagreement still exists surrounding seed oils not just in the public discourse, but among scientists themselves.
[embedded content]
Several years ago, I attended a large international nutrition science conference where one session in particular caught my attention. The session was titled: “Why Omega-6 Fatty Acids Are Good for Health.” The wording struck me as odd. Omega-6 fatty acids are the main component of seed oils. The session wasn’t framed as a question “Are seed oils good or bad?” but instead as a defense of their health benefits. That assumption felt premature. We were gathering as scientists to explore evidence and challenge accepted thinking, yet the session title suggested preconclusion. When the presentations began, the speakers largely focused on how omega-6 fatty acids reduce LDL (“bad”) cholesterol, a commonly accepted surrogate marker for heart disease risk. What the session didn’t address in depth was whether long-term, high consumption of seed oils truly results in better health outcomes, or whether the mechanistic link between omega-6 levels and disease risk might be more complex.
This conference experience was just one example, but it reflected a broader tendency in the nutrition science community to simplify public health recommendations. To be clear: I am not saying that seed oils are “bad.” I’m saying we don’t know. That’s why I don’t eat food made with seed oils myself, as I’m not sure what the causal effect is. It is my personal choice, you may agree or not agree. As it stands now, the only conclusions we can draw from the scientific evidence is to be cautious, especially when we are talking about mass consumption of a food component that was virtually absent from the human diet 100 years ago.
The truth is, we don’t fully understand what the causal effect of omega-6 fatty acids is, which dominate most seed oils, on disease risk.
While traditional observational studies often link omega-6 intake to better cardiovascular outcomes, these studies come with well-known limitations: People who consume more seed oils may also engage in other healthy behaviors that confound the results. History offers many cases — such as vitamins A, D, and E — in which repeated observational benefits were later contradicted by randomized controlled trials (RCTs), the gold standard for establishing causality. For example, evidence from observational studies show that dietary vitamin A intake was related to lower cardiovascular risk, but a large RCT in 11,036 participants showed no benefit.
In the case of omega-6 fatty acids, both RCTs and Mendelian randomization (MR) studies — a genetic epidemiology method used to infer causality — paint a more mixed picture. Evidence from MR suggests that higher endogenous omega-6 levels have no benefit on heart disease. Of course, MR is not perfect, either. Every study comes with limitations. However, the MR evidence echoes findings from RCTs. For example, the Minnesota Coronary Survey, a large RCT conducted in 1968-1973 with over 9,000 participants, showed that cholesterol lowering by replacement of saturated fat with vegetable oil rich in linoleic acid did not lower the risk of coronary heart disease. Meta-analyzing this study with other clinical trials also showed no benefit. Taken together, these findings suggest that the case for seed oils as unequivocally “heart-healthy” is not closed.
Seed oils are everywhere in the modern food supply. Fast food, packaged snacks, salad dressings, and even so-called “healthy” foods often rely on soybean or corn oil as the primary fat. According to a study using data from USDA, Americans get around 8% of their daily calories from linoleic acid, the primary omega-6 fat in seed oils, a massive jump from early 20th-century levels. Yet we’ve only scratched the surface in understanding what sustained intake at these levels means for long-term health.
The scientific community should be honest about this uncertainty. It’s OK to say: “We don’t yet have all the answers.” Doing so doesn’t confuse the public; it respects them. It signals that we’re still asking questions and are open to new evidence, even if it challenges longstanding beliefs.
Until we know more, we should be cautious about making sweeping recommendations. In the meantime, the best advice may be this: favor balance over extremes. That means not fearing every bite of croissant, but also not assuming that loading every meal with seed oils is a surefire path to good health.
The seed oil debate doesn’t need more hype — it needs more humility. And more science.
Jane Zhao, a Takemi fellow at Harvard and assistant professor at the University of Hong Kong, has more than 10 years’ experience researching the causal effects of dietary factors and medications on chronic diseases.